Painful sex, explained: Doctor and patient break down a taboo women's health topic
Callista Wilson, a San Francisco mom of a 2-year-old, experienced pain the very first time she had sex with a man.
Wilson, now 40, didn't speak for years to anyone about her experiences with painful sex, and she didn't get medical help for it until more than a decade later, after countless doctor visits.
"I really blamed myself," Wilson told "Good Morning America." "And I think that's kind of a common response."
Also common is how many women experience painful sex. Nearly three out of every four women experience pain during intercourse at some time during their lives, according to the American College of Obstetricians and Gynecologists (ACOG).
Even so, Wilson said she struggled to find information about painful sex online, was not having those types of conversations with her friends and often felt like she was not taken seriously by doctors.
At one point, Wilson said she was told by a physical therapist that she was just going to have to "live with it" for the rest of her life.

"The message I was getting from doctors was that, 'You're imagining all of this,' or, 'You're making this up, and we don't believe you, and you can't talk to us about this,'" she recalled. "And so I really just continued to hold it all inside."
Years later, Wilson finally opened up to a long-term boyfriend about the pain she experienced during sex, an honest conversation that ultimately led to their breakup. For Wilson and so many women, painful sex is not just a painful experience physically, but also one that can be emotionally and mentally devastating.
It was affecting my whole life
"All that time, it wasn't just like sex hurts. It was like, sex hurts. You can't be in love. You'll never have children. You're a broken woman," Wilson said. "It was affecting my whole life. Every facet of my life."
It wasn't until her early 30s that Wilson felt comfortable opening up to a close group of friends about how painful sex was for her. She remembers it was her friends who told her, "You cannot settle for this."
At their urging, Wilson saw a specialist in New York City, an OB-GYN whose specialties include sexual pain disorders.
The doctor diagnosed Wilson with congenital neuroproliferative vestibulodynia, a type of chronic pain in the area surrounding the vaginal opening, according to the National Vulvodynia Association, a nonprofit organization that advocates for women's health.
Because the type of surgery required to treat vestibulodynia was not covered by Wilson's insurance, she delayed the surgery for one year in order to save nearly $20,000 to cover the costs and required time off of work.
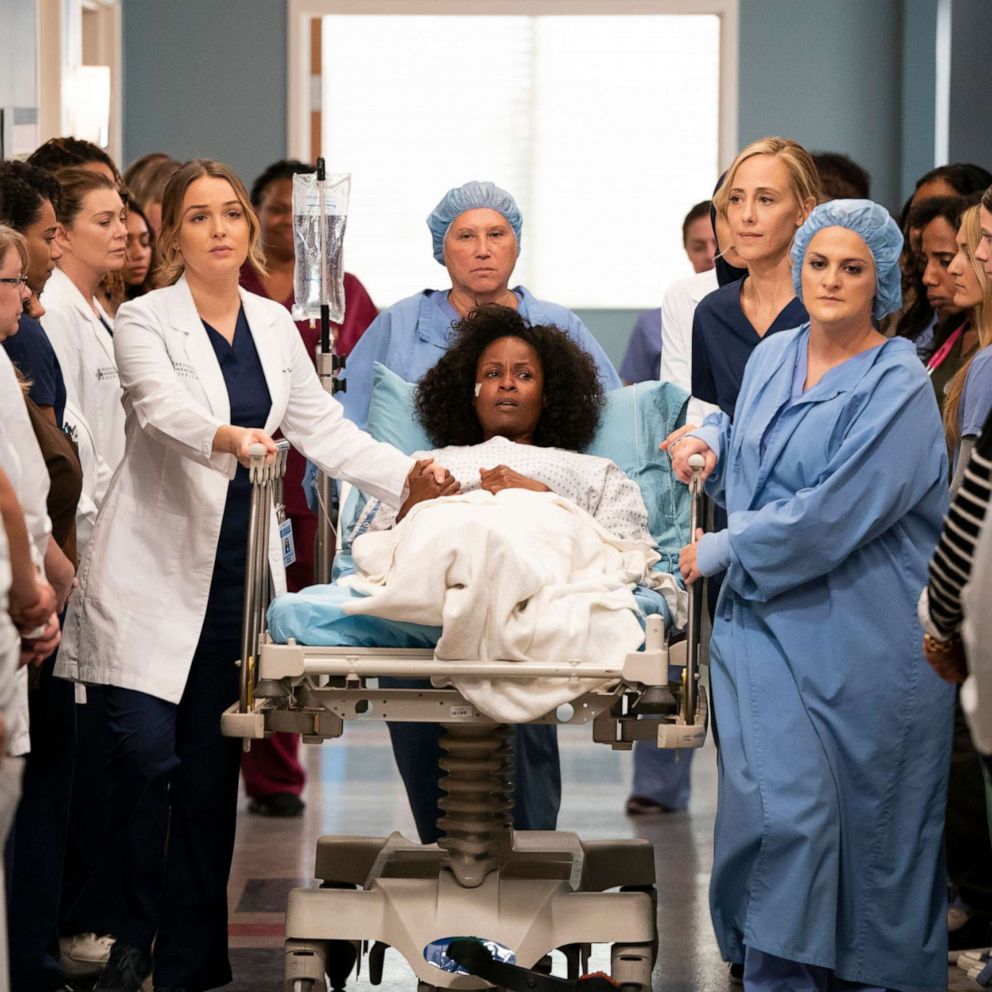
At age 35, after a nearly two-decade search for answers, Wilson was treated successfully for her condition.

Two years ago, Wilson gave birth vaginally to her son, something she never thought she would be able to do.
"Once I healed from my surgery, my life began," she said. "I used to joke I was 35 going on 15 because that was kind of how it felt, like I get another chance at this."

Why did the topic become so taboo?
Much like childbirth or menstruation, painful sex is something that so many women go through but don't talk about with their friends or even with their doctors.
"Somewhere along the way, it was decided that this was a 'taboo topic,' when it shouldn't be a taboo topic at all," said Dr. Nita Landry, a Los Angeles-based, board-certified OB-GYN. "And in some instances, it's that providers don't feel comfortable talking about it."
Women often have a hard time getting an accurate diagnosis for painful sex and vaginal pain, which often contributes to the stigma, according to Landry.
GoodMorningAmerica.com is tackling a different taboo women's health topic each month, breaking down stigmas on everything from mental health to infertility, STDs, orgasms and alcoholism.
"[Women] feel like there isn't hope so they kind of stop talking about it and they learn to live with it, or they talk to a provider who tells them, 'Oh, you're just going to have to learn to live with this,' and then they don't take it any further," she said. "And that's how they spend the rest of their lives."
Wilson said once she had a specific diagnosis, "everything changed" for her in terms of how open she felt speaking about her pain.
"Prior to having a diagnosis, it was much harder to be open and to share, because it was still this kind of ambiguous thing that I didn't understand," she said. "Once I had the vocabulary, my voice, I couldn't stop it. I told everybody."
And once she started speaking out about her experience, Wilson said she felt a kind of "collective healing" as she received messages on social media from women around the world.
"For so many years I had felt like I was the only person suffering from this and that I was all alone," she said. "But there are so many women out there who are in this boat, and we're all here together and just raising our voices."
What people need to know about painful sex
Painful sex is something anyone could experience, no matter their gender or sexual orientation, according to Landry.
But, it is not something that people should have to endure, because there are solutions, she noted.
"If you are having sex, as long as it's consensual, you deserve to have good sex," she said. "Your sexual orientation or your gender identity, that doesn't matter. You should be able to talk to your partner or your health care provider, because [everybody] deserves good sex."
Persistent or recurrent discomfort that happens just before, during or after sexual intercourse
Painful sex, known medically as dyspareunia, is defined as persistent or recurrent discomfort that happens just before, during or after sexual intercourse. It also includes pain during other sexual activities, like any type of stimulation of the clitoris, vagina, vulva and perineum (the area between the anus and the vulva), according to Landry.
During sex, for those with dyspareunia, pain may be felt in the vulva, within the vagina or the perineum or in the lower back, pelvic region, uterus or bladder, according to ACOG.
Some women may also feel pain when they insert tampons or undergo a gynecological exam, as was the case with Wilson's condition.
"It's important to realize that different people will describe that pain differently," Landry said. "For instance, some people will experience pain with penetration, whereas other people will have pain with deep thrusting. Some people describe their pain as sharp or burning, whereas others have more of a crampy pain."

"At the end of the day, it just means that it is uncomfortable for you," she said.
Causes of painful sex
While there are many symptoms of painful sex, there are also many causes, some physical and some psychological, according to Landry. When going to a health care provider about painful sex, the provider will want to take a detailed history and do a physical exam.
"I can't tell you how many patients will say, 'I'm having painful sex,' and I ask them about their relationship, and they say, 'You know, it's not that good,'" she said. "That's going to play a huge role in how much you're going to enjoy sex, or it could be anxiety, depression, a history of sexual abuse."
In those cases, a woman would want to reach out to their health care provider as well as a mental health care provider, experts say.
Pain during sex may be a sign of a gynecologic problem, such as ovarian cysts or endometriosis.
It can also be caused by everything from skin disorders and hormonal changes to tears in the perineum caused by childbirth, sexually transmitted diseases, inflammation of the vagina, vulvodynia (a pain disorder in the vulva) and vaginismus (tightening of the muscles at the opening of the vagina), according to ACOG.
"You definitely need to see a qualified health care provider so you can figure out what's going on," Landry said. "You could be in a situation where there's an underlying medical condition that needs to be treated, or you may be in a category where you don't have an underlying condition that's really going to have a negative impact on your health, however, it's having a negative impact on you because you're having painful sex."
Treatments for painful sex
Not every woman experiencing painful sex is going to need to undergo surgery, as Wilson did, according to Landry.
"The big thing to remember is your treatment is going to depend on what's causing your painful sex, and because there can be so many different causes, the treatment plans can vary greatly," Landry said. "A lot of times, your health care provider can help you find your treatment option that is non-surgical, and that's ideal."
In cases where there is an underlying condition, like a sexually transmitted infection, doctors are going to treat the underlying condition first. In cases where there is not an identifiable cause for painful sex, doctors will likely try therapies such as a topical anesthetic applied before and after intercourse or pelvic physical therapy, Landry explained.
"Honestly, it may take some time," she said. "It's not necessarily you'll do something on a Monday and on Tuesday you'll be all better all the time."
Women in particular need to take steps to make sure they are working with a health care provider that takes their concerns of painful sex seriously, Landry noted.
"If you feel as though you're being dismissed, if you feel like they are not taking your complaint seriously, then you need to find another provider," she said. "Just know that there are providers out there who want to talk to you about this."
GoodMorningAmerica.com is tackling a different taboo women's health topic each month, breaking down stigmas on everything from mental health to infertility, STDs, orgasms and alcoholism.