Americans who haven't had COVID-19 are now in the minority following omicron surge
A new CDC analysis estimates that at least three out of every five Americans have antibodies that indicate a prior COVID-19 infection. Before the omicron-fueled surge in cases from December 2021 to February 2022, only an estimated one-third of people in the U.S. were estimated to have a prior infection.
"This is the first time that population seroprevalence is over 50%," Dr. Kristie Clarke, co-lead for the CDC's COVID-19 Epidemiology & Surveillance Taskforce Seroprevalence Team, told reporters on a press call this afternoon.
Clarke said she had expected a post-omicron increase in seroprevalence -- antibodies that show previous COVID-19 infection -- but not this much of an increase.
An average of 58% of people across all age groups had detectable antibodies as of February -- but that rose to nearly 75% among children and teens under 17.
"We had 43% in January and I did expect it to increase. I didn't expect it to increase quite this much, but we follow the data and we look at the data and this is what the evidence is showing us and so this is why we want to get this message out to the U.S. population as soon as possible," Clarke said.
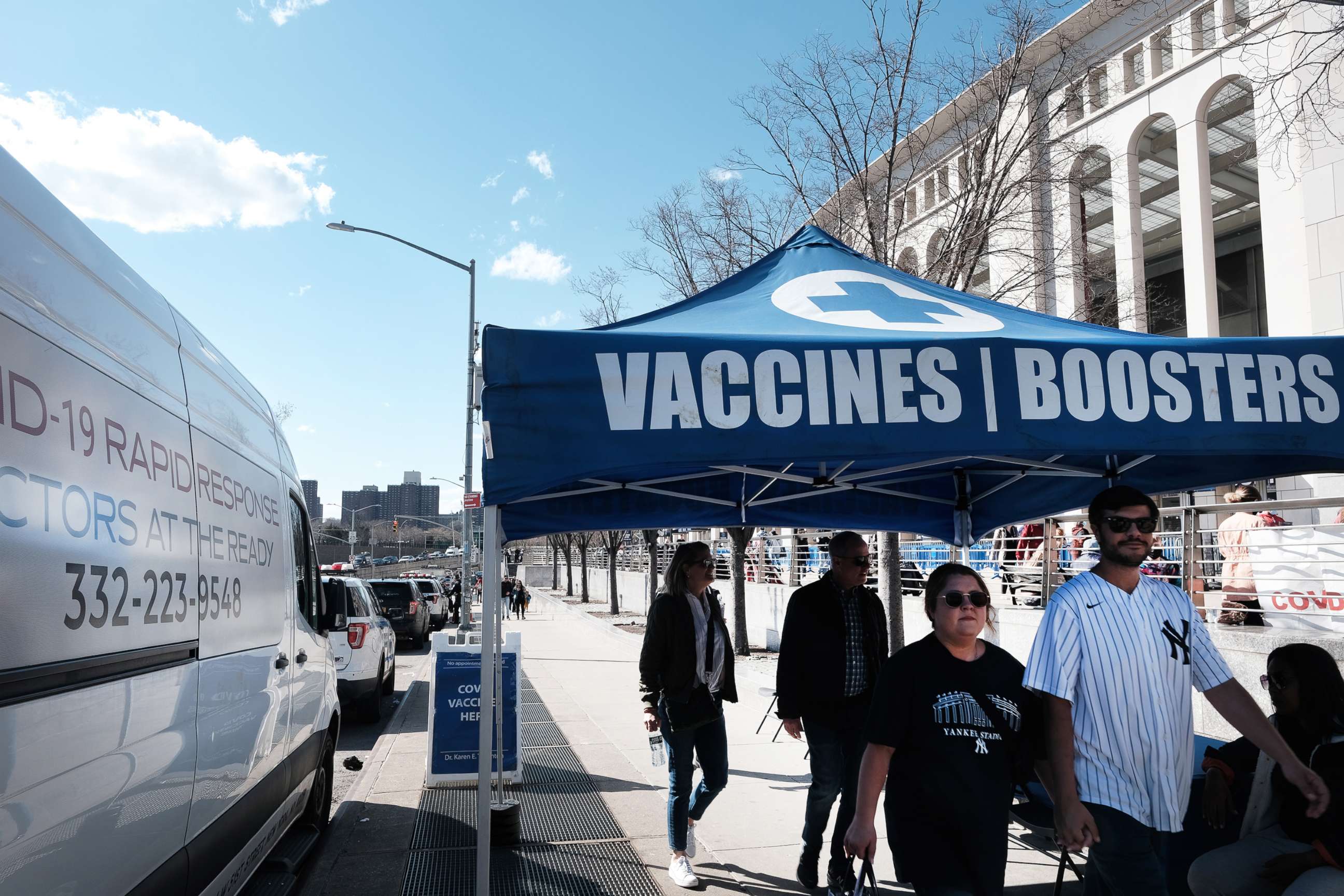
The jump in antibody protection, both from infection and from vaccines and boosters, is part of the reason why the CDC went ahead with its recent decision to use new metrics for masking and community warnings, CDC Director Rochelle Walensky said.
"We do believe that there's a lot of protection in the community both from vaccination as well as from boosting and from prior infection," she said.
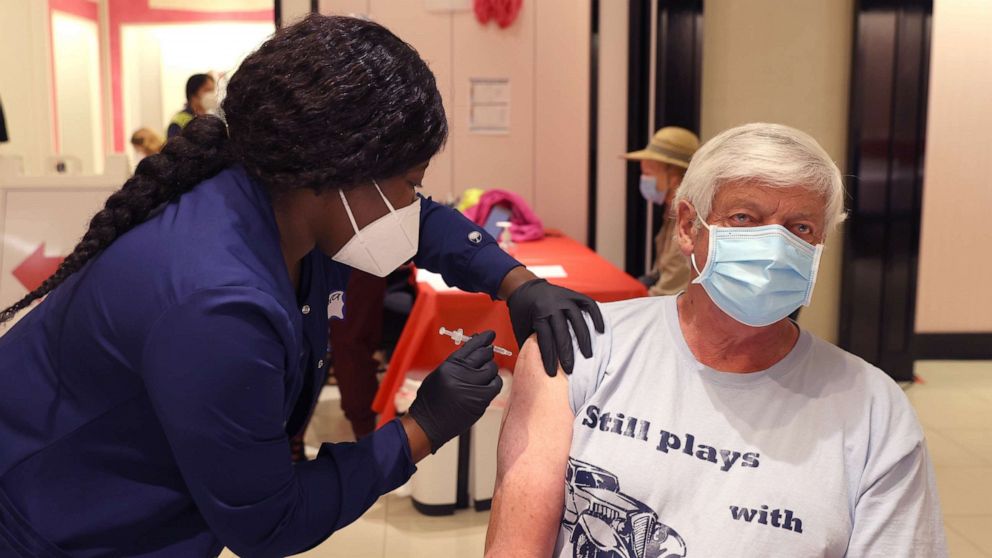
But Walensky and Clarke repeatedly emphasized how important vaccination still is. There's very little information on how long immunity from a case of COVID lasts, but a lot more data on how long immunity from vaccines and boosters lasts.
"I can't underscore enough what Dr. Clark said, which is those who have detectable antibody from prior infection, we still continue to encourage them to get vaccinated," Walensky said.
"We don't know ... when that infection was, we don't know whether that protection has waned. We don't know as much about that level of protection than we do about the protection we get from both vaccines and boosters," Walensky said.
Clarke said this study cannot be interpreted to mean 60% of Americans have protection against reinfection.
"Reinfection happens and infection after vaccination can happen," Clarke said.
Nor does the percentage mean we've reached some kind of herd immunity, she said.

"There's also no known threshold of the population where once you get above X percentage will completely stop community transmission of COVID. So all of that is really important to know," Clarke said.
Still, there is continued good news on the BA.2 variant, which has yet to cause a significant jump in severe illness or death, Walensky said, though there are a few counties in the Northeast that the CDC now categorizes as medium or high risk, which are recommended for masking indoors.
"There are some areas of the country, particularly in the Northeast, where we're seeing higher number of cases and we're starting to see some hospitalizations tick up. You know, we're watching this carefully," Walensky said.
But she noted: "We haven't seen them tick up as much as we might have expected in prior times during this pandemic, thanks to, I believe, a large amount of protection in the community both from disease and infection, as Dr. Clark has articulated, as well as vaccine protection."
The hospital stays that the CDC is monitoring have also not been as severe as in the past, she said.
"We're seeing less oxygen, use less ICU stays. And we haven't, fortunately, seen any increase in deaths associated with them. So we are hopeful that positive trends will continue that we will not see as a result of these increasing cases, any further severity of disease," Walensky said.