New recommendations to offer more women risk assessment for BRCA-related mutations – that can include breast cancer
Annually, about 247,200 cases of breast cancer are diagnosed in the U.S. and nearly 42,000 people die each year from breast cancer, according to the Centers for Disease Control.
Besides certain types of skin cancer, more women are diagnosed with breast cancer than any other cancer in the U.S., regardless of race or ethnicity.
The United States Preventative Services Task Force (USPSTF), an independent, volunteer panel of national experts in prevention and evidence-based medicine which most doctors follow, has expanded its recommendations for screening for BRCA1 and 2 gene mutations, "some of the most common gene mutations seen in inherited breast cancers," Dr. Banu Arun, professor of Breast Medical Oncology and co-director of Clinical Cancer Genetics at the University of Texas MD Anderson Cancer Center, told "Good Morning America" in an interview.
Before today, women with a family history of certain types of cancer were encouraged to have additional screenings for a risk assessment that may predispose them to being diagnosed with breast cancer. The updated recommendations now also looks at the woman’s personal medical history and will encourage additional risk assessment if she has concerning risk factors herself.
Women who have "had breast, ovarian, tubal, or peritoneal cancer and have not been tested or who have ancestors associated with BRCA1/2 gene mutations" should also be assessed for risk, Dr. Carol Mangione, task force member and professor of medicine and public health at UCLA, told "GMA."

There are several quick risk assessment tools that health care providers can use. If it is positive, the final USPSTF recommends "genetic counseling and, if indicated after counseling, genetic testing."
"We do not recommend routine assessment of people who do not have a personal or family history or ancestral connection," Dr. Mangione said. "The harms of doing so outweigh the risks."
If doctors "implement these recommendations in their routine clinical practices it will increase patient and provider awareness. More patients will be tested and we will miss less," said Dr. Arun.
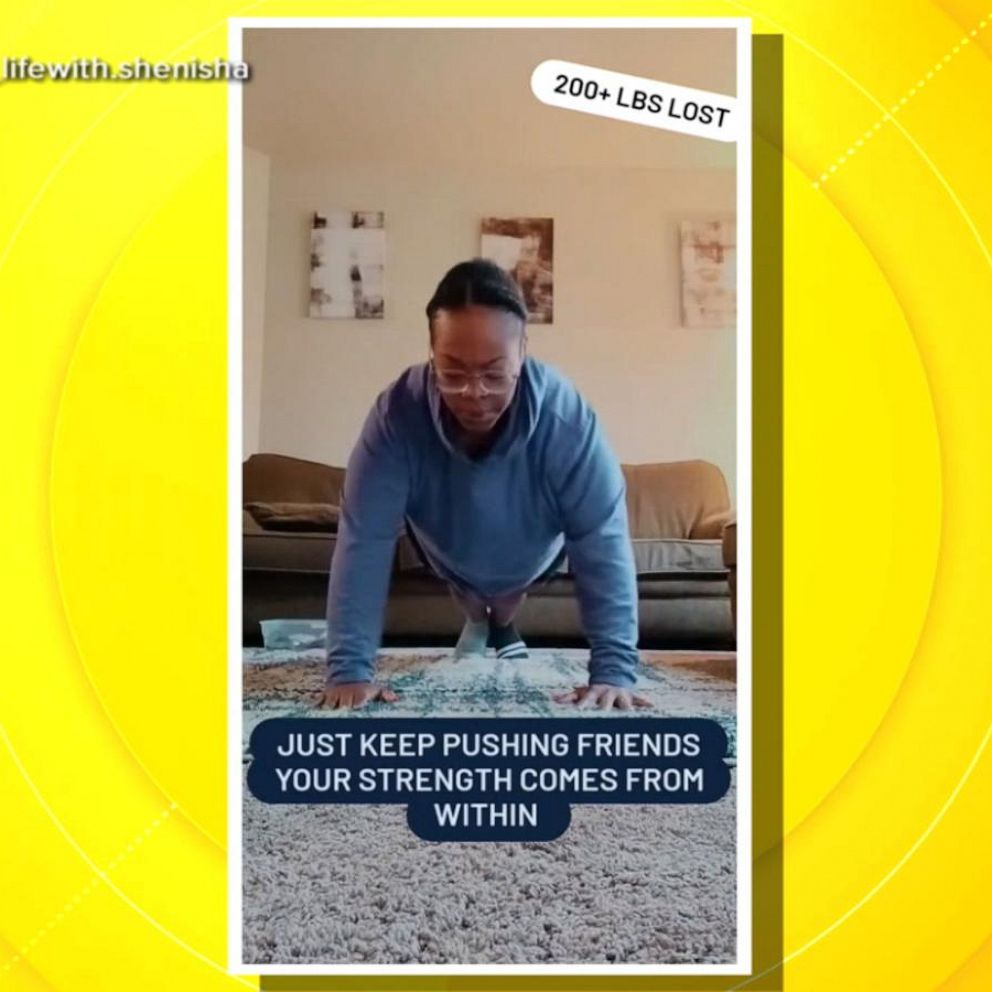
Dr. Arun recommends, "Knowing your family history, living a healthy lifestyle, engaging in physical activity, and having proper weight control" to help reduce the risk of developing breast cancer.
However, the new recommendations, do not "address many persistent problems," according to Dr. Susan Domcheck, executive director of the Basser Center for BRCA at the Abramson Cancer Center at the University of Pennsylvania, who released an editorial published in JAMA. The changes are "certainly valuable," she commented in a Penn Medicine news release, but "they do not include newly diagnosed breast or ovarian cancer patients or advanced cancer patients in its recommendations."
Dr. Domcheck and the USPSTF indicate the need for additional research regarding BRCA mutations and risk factors, including the effect of race, ethnicity and socioeconomic status.
Kimberly Dike, M.D., is a senior internal medicine resident at the University of Texas Health Science Center at Houston, working with ABC News Medical Unit.