Breast cancer care becomes troubling casualty of COVID-19 pandemic
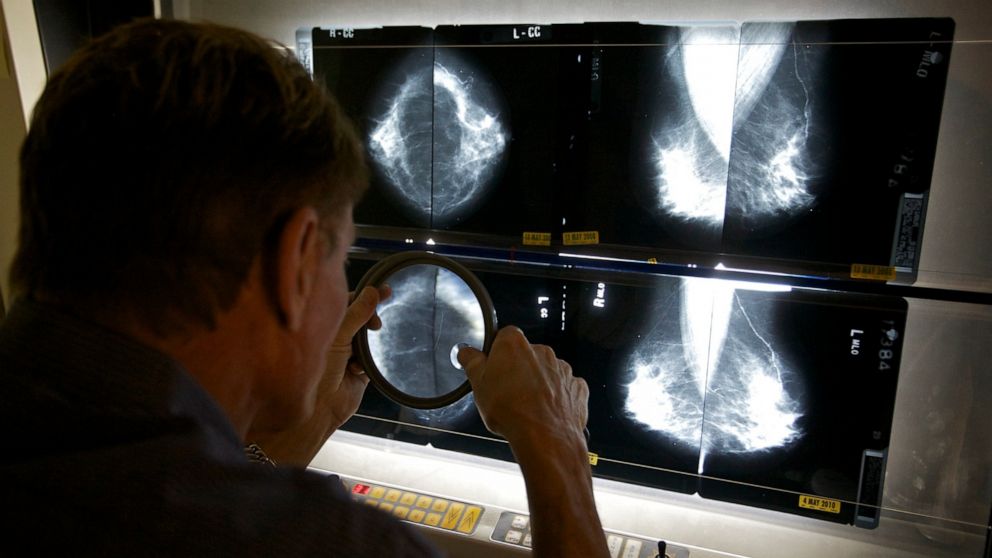
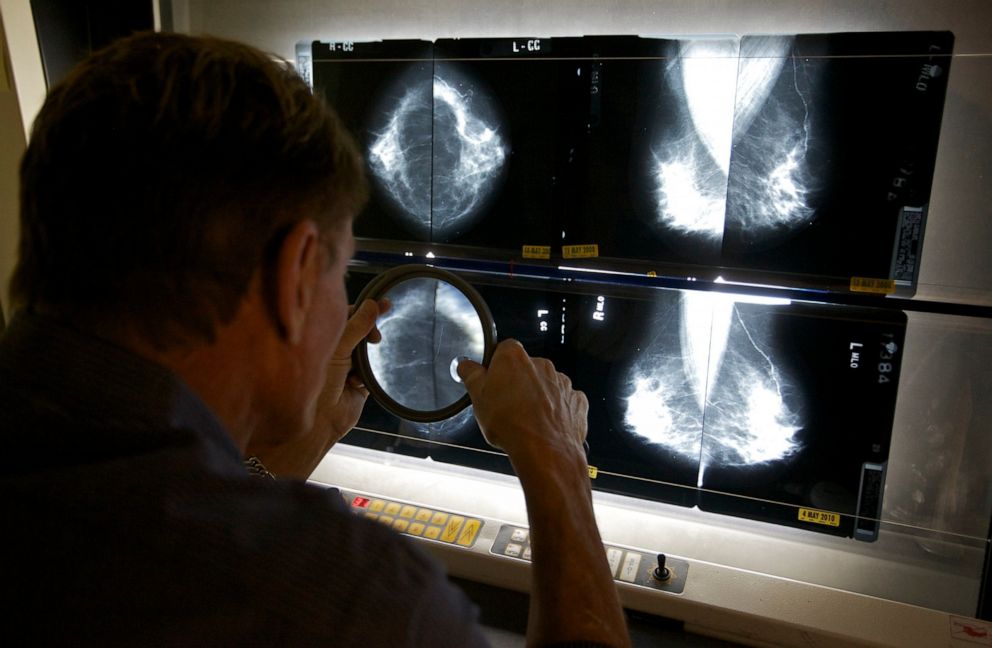
As many hospitals and doctor's offices limited patient appointments and surgeries during the coronavirus pandemic, a concerning side effect of the shutdown began to emerge. With fewer screening exams, patient visits and surgical procedures, breast cancer care took a frightening hit.
Regular breast cancer screenings save lives, but early in the pandemic, the American Cancer Society recommended that doctors postpone any routine breast cancer screenings or intervention to protect at-risk patients from potential exposures or illness.
"No one should go to a health care facility for routine cancer screening at this time," Dr. Richard Wender, chief cancer control officer for the ACS, said in a statement on April 29.
But delaying those appointments didn't just mean delaying regular breast exams. For some, it meant delaying preventative treatments, such as chemotherapy, designed to keep cancer from coming back. And as weeks turned into months, ACS eventually shifted its policy, encouraging women to talk to their doctor before potentially resuming their regular appointments.
The most recent statement, released on July 2, encouraged women to resume their usual screening mammograms, but suggested that some women can choose to wait for two years for their next screening mammogram based on their individual history and breast cancer risk factors.
Though the earlier advice has now changed, we don't know the effect these delays might have on breast cancer patients in the future.
Dr. Paulomi Shroff, a board-certified breast surgeon in Marietta, Georgia, has experienced the impact of the shutdown on her patients firsthand.
"Originally, an issue was that we couldn't get mammograms for about six weeks in Georgia," she said. Many other places around the country had even longer delays meaning that "women who had breast lumps would get pushed back in terms of getting them investigated."
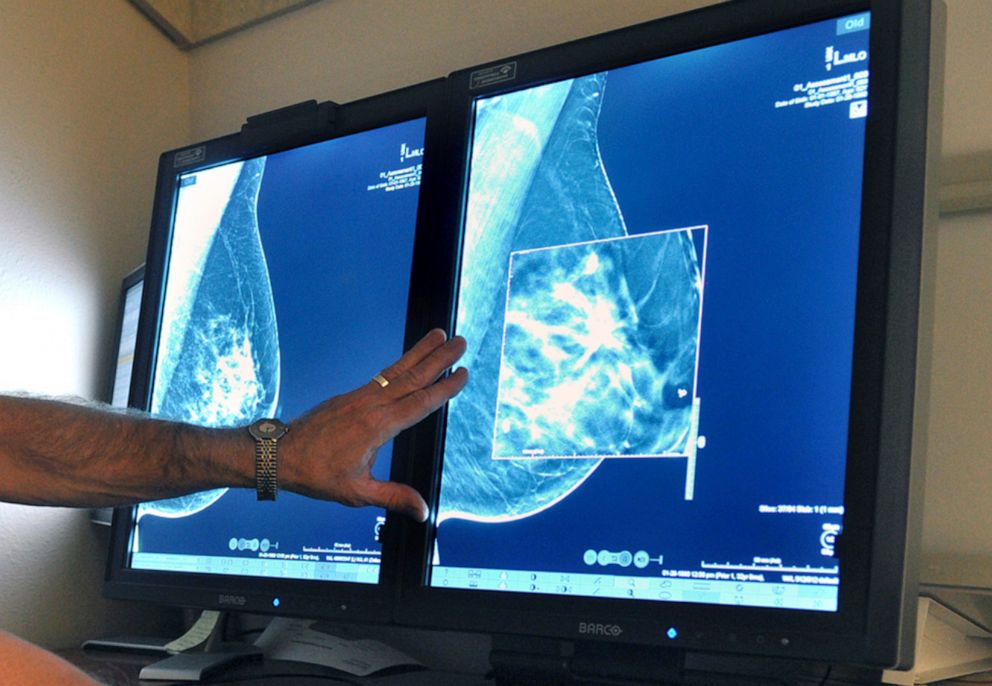
Stopping mammograms did not just affect the women with breast lumps. Shroff said that it also affected women scheduling their yearly mammograms to screen for breast cancer.
"Really the problem with not having mammography in that time period is that women are skipping their mammograms," Shroff said. Because many women make a habit of getting their mammograms at a certain time of year, "if they were supposed to have their mammogram in May and didn't get it, they may just wait until next May," she added.
Altogether, the delays in mammograms could mean even more trouble for women down the road.
For patients diagnosed with breast cancer before the pandemic, the shutdown impacted their access to physicians, medications and surgeries. "A lot of different centers de-prioritized breast surgery," Shroff said.
This is a concern, she said, because by performing surgery "as early as possible, we are reducing the metastasis risk."
While patients waited for surgery, some who had certain types of cancer could be prescribed medications that would help keep their cancer from worsening.
Once elective surgeries were resumed, the pandemic had an impact on the decisions women made for having their breast cancers removed. In an effort to conserve hospital beds and to avoid overnight hospital stays, many patients and surgeons opted for less-invasive surgeries.
"In patients who might have otherwise wanted a mastectomy, if we could get away with a lumpectomy, we got away with a lumpectomy," Shroff said.
For those considering having a plastic surgeon reconstruct their breasts after having their breast cancers removed, Shroff said, "If they needed reconstruction we tried to do the minimum possible" to avoid an overnight hospital stay.
Even for patients without cancer, but with a high-risk change in their breast tissue called atypia, the pandemic caused problems. Shroff told ABC News that she had one patient with atypia who had to wait three months for surgery. By the time she had her surgery, it had progressed into cancer.
"I effectively sat on it without treatment for three months, which is not something I would have done in a non-COVID era," Shroff said.
Fortunately, multiple national societies are providing guidance to doctors making decisions about breast cancer care.
"Our society, along with four other societies ... wrote really literature-based guidelines about what to do with breast cancer patients during the pandemic," said Dr. Jill Dietz, president of the American Society of Breast Surgeons.
In addition to recommendations for virtual visits, streamlined in-person visits, masks, screening and preoperative testing, the guidelines prioritize patients' cancer care based on their individual risk of breast cancer progression or of serious illness should they contract COVID-19. Dietz said, "All of those factors are playing a role."
In terms of resuming mammograms, Dr. Lynn Baxter, director of breast imaging for Northside Radiology Associates at Northside Hospital in Atlanta, said that even though mammograms are back up and running at her facility, not everyone should be rushing to be seen.
"Let's say someone is older and has COPD -- if it's just a regular screening, it might be in the best interest of her health to wait. ... Let's say that same lady felt a lump, I would say, no, she really needs to come in and get that taken care of."
Most importantly, Baxter recommended that women "think about their individual risk and talk with their providers."
Along with these prioritization strategies, Shroff wants women across the country to know: "You don't need to be scared to go the doctor's in the pandemic, as long as you practice good personal hygiene, wear a mask, wash your hands. Don't not seek medical care because of this."
Stephanie E. Farber, M.D., is a plastic surgeon in Atlanta and is an ABC News Medical contributor.