Why Blood Transfusions From Ebola Survivor Dr. Kent Brantly Could Help Patients
— -- Ebola survivor Dr. Kent Brantly has donated the plasma in his blood to three patients in the last month, echoing what one of his former patients did for him before he left Liberia.
Brantly was caring for sick Ebola patients with the aid group Samaritan's Purse in Monrovia, Liberia, when he became the first American diagnosed with Ebola in late July. His condition was worsening before he was flown to the United States in an air ambulance, but before he left, one of his former patients, a 14-year-old Ebola survivor, gave him "a unit of blood" for a transfusion, according to Samaritan's Purse.
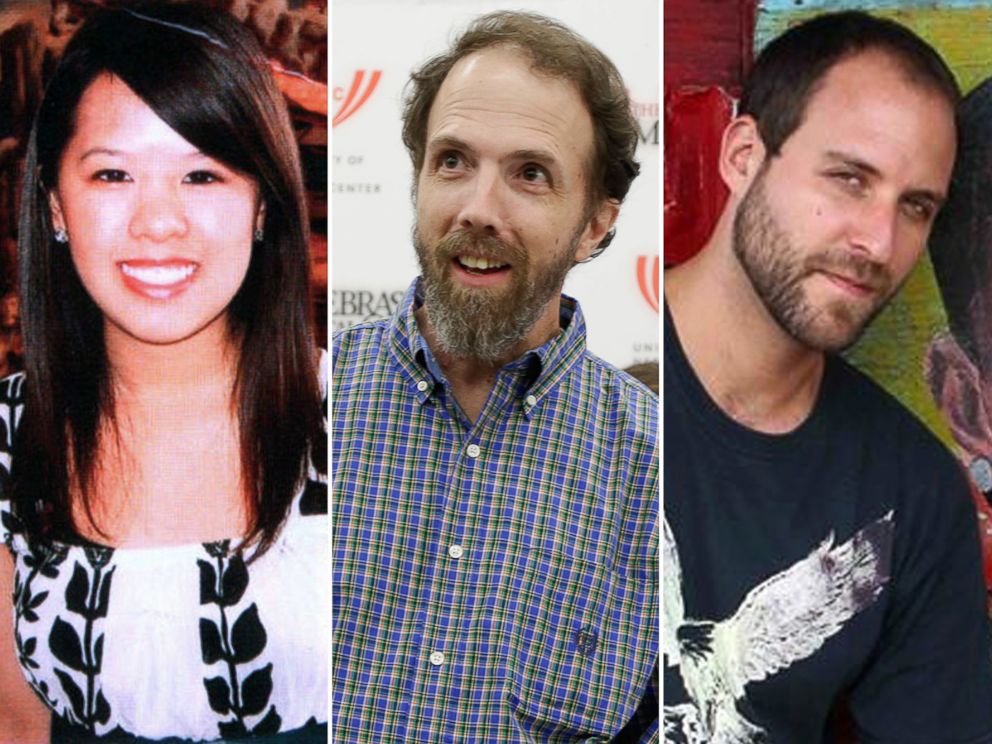
Since his recovery and release from Emory University Hospital on Aug. 21, Brantly has donated his plasma to Samaritan's Purse colleague Dr. Rick Sacra and freelance cameraman Ashoka Mukpo, both of whom were receiving treatment for Ebola at Nebraska Medical Center. They received his plasma transfusions on or around Sept. 11 and Oct. 8, respectively -- about 27 days apart. The latest American Ebola patient, Dallas nurse Nina Pham, who contracted the virus while treating Thomas Eric Duncan, received a blood donation of some kind from Brantly, according to health officials.
Plasma is a component of blood that contains virus-fighting proteins called antibodies. When someone donates plasma, their blood is drawn into a machine that separates out the plasma and returns the red blood cells to the donor.
"There is a strong theoretical possibility that this could help, particularly if this is given early," said Dr. William Schaffner, chair of preventive medicine at Vanderbilt University Medical Center in Nashville, Tennessee.
Here's how it works: When confronted with a virus, the immune system creates antibodies to specifically target that virus, kill it and keep it from coming back, he said. Once a person has antibodies, they stay in their blood for life. If the Ebola antibodies found in an Ebola survivor's blood can be imported into struggling Ebola patient's body, those antibodies can theoretically help the patient's immune system fight off the deadly virus.
"What those antibodies do is bind to the virus," Schaffner said. "They find the virus and bind to it and prevent it from multiplying further."
Schaffner said even though the sick person's body is trying to make antibodies, an infection can be so overwhelming that the sick person's immune system might not be able to keep up with the invading virus. As a result, the sooner someone gets a plasma transfusion, the more likely it is to help that person recover, he said.
During his battle with Ebola, Brantly also received the experimental drug ZMapp, a cocktail of three synthetic antibodies to attack Ebola, before leaving West Africa for Emory University Hospital. Brantly was declared virus-free and discharged on Aug. 21, but the hospital epidemiologist, Dr. Bruce Ribner, said it wasn't clear what roles ZMapp and the transfusion played in his recovery.
A person can donate plasma up to 13 times a year, or every 28 days, unlike whole blood donations, which must be spaced between two and four months apart, according to the American Red Cross. Though Brantly's first two plasma donations were spaced about a month apart, his last two were barely a week apart. But it's also possible Brantly donated excess plasma during one of his donations, which then went to Pham.
Though blood type O is considered the universal donor for whole blood, type AB is the universal donor for plasma, according to the Red Cross. According to Texas Health Presbyterian Hospital, where Duncan was being treated, Duncan did not receive any kind of blood transfusion because his blood type was not compatible with any of the donors.
In September, the World Health Organization said blood therapies should be "considered as a matter of priority." Since then, the number of people who have been infected with Ebola since March has doubled to 8,399, and 4,033 of them have died, according to the latest WHO figures.
"There is a real opportunity that a blood-derived product can be used now and this can be very effective in terms of treating patients," said Dr. Marie Paule Kieny, WHO's assistant director general, said on Sept. 5.




