An urgent mental health crisis: Health workers facing immense psychological toll from pandemic
Dawn seems to be breaking in the COVID-19 pandemic. As vaccines provide new hope, cases and hospitalizations have been declining across the country. But as one calamity gradually wanes, another silent crisis is making its way out of the shadows.
Experts say some doctors, nurses and other health workers on the frontlines will have to face a mental health reckoning after being in the trenches fighting the global pandemic.
“We will continue to fight, but we’re exhausted and we’re tired and -- mentally, physically, emotionally -- just worn down,” Jerusha Robinson, an intensive care unit nurse in Tennessee, told ABC News in a video diary.
Kelsey Copely, a respiratory therapist from Minnesota, echoed that sentiment.
“It’s hard for us health care workers," she told ABC News. "I’ve seen more deaths these past few months than I had seen in years, and it’s not normal and it takes a lot. It takes a toll on someone’s mental health.”
Health care professionals like Copely and Robinson have forged forward amid unparalleled obstacles as they've fought to save lives. Too often over the last year, they've been the bridge in heart-wrenching moments when families are forced to say goodbye to loved ones -- sometimes over the phone.
“The pandemic has had a terrific strain on nurses,” Dr. Ernest Grant, president of the American Nurses Association, told ABC News.
Dr. Susan R. Bailey, president of the American Medical Association, told ABC News in a statement: “Acute stress among physicians, which was already significant before the pandemic, has increased dramatically for many physicians during the last several months as the pandemic has brought new challenges and exceptional demands.”
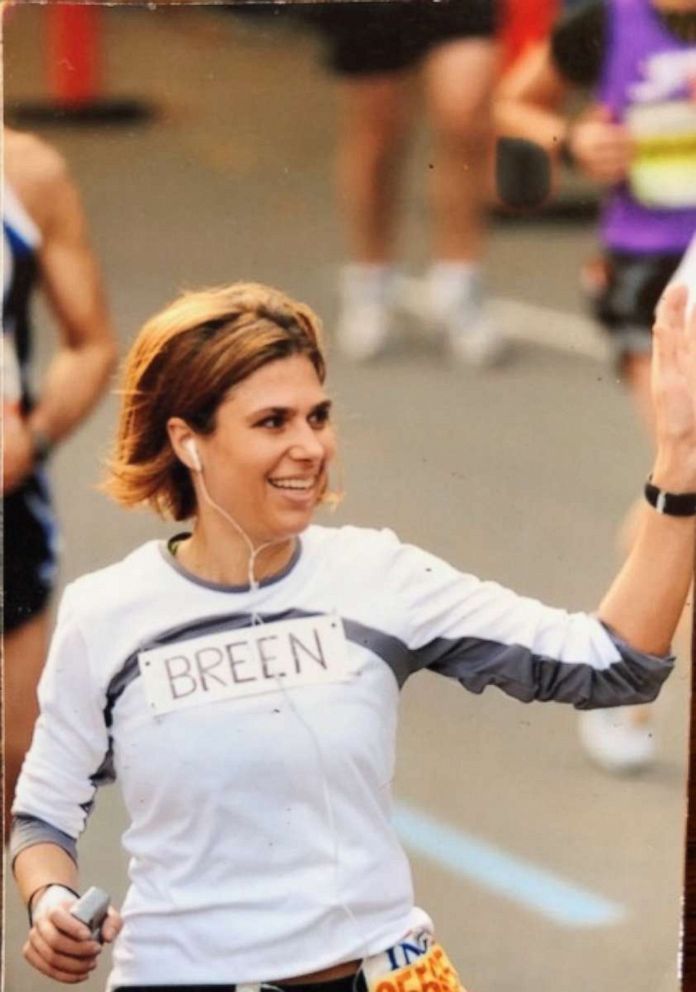
Dr. Lorna Breen, medical director of the emergency department at New York-Presbyterian Allen Hospital, died by suicide in April 2020, just a couple of months after the virus began spreading widely across the U.S. Her family says the weight of the unrelenting pandemic crushed her seemingly indomitable spirit.

“My sister Lorna was just a rockstar," Jennifer Feist, Breen's sister, told ABC News. "She was super smart, super driven. ... She was a very active snowboarder ... [had] tons of friends in New York. Just living the dream."
Breen’s family says she hadn't previously exhibited signs of mental health distress.
“Not once. That’s what makes this entire experience so absolutely outrageous and unbelievable,” said Feist.
Feist said the confluence of tragedy, exhaustion and death was the tipping point.
“You take away the sleep, you take away the rest, you compound it with a deluge of people, many of whom are dying. And again, at that time, nobody knew what to do with this virus. This was the very beginning,” said Feist.

Breen's death was a devastating blow and shock to those who knew her best.
“It happened very quickly and when I say quickly, I mean in days it happened. This can happen to other people and we need to pay attention and we need to be vigilant,” Feist said.
Breen’s family says her case underscores an urgent need for a mental health reckoning in hospitals across the country.
Prior to the pandemic, an estimated 300 to 400 physicians died by suicide annually, which equates to one physician per day, according to research presented at the 2018 American Psychiatric Association meeting.
At this time, experts say there is still not enough data to assess the psychological toll COVID-19 has had on physicians in the past year.
“It was very clear that physicians did not know how to reassure themselves or take care of their mental health,” Mona Masood, D.O., an outpatient psychiatrist working in Philadelphia, told ABC News.

In March, 2020, Masood created the Physician Support Line, a free, confidential service to give doctors a mental health outlet during the pandemic. To date, Masood said a team of 700 volunteer psychiatrists has already provided support to more than 2,000 physicians and medical students.
“For me, as a psychiatrist, it became the writing on the wall that if we are not able to keep our heads above water, how are we going to be able to take care of the many people that would eventually need us," Masood said.

Kentucky-based physician Dr. Genevieve Jacobs called into the service during a time of consuming stress. She said just one call gave her the support she needed.
“I called and a physician picked up right away," she said. "So I was, first of all, surprised that it works. It was nice to have someone to talk to that was outside of [my] place of work... It’s not something that’s going to be brought up or you don’t think that person’s thinking about it when you’re having lunch with them the next day.”

Masood says it’s essential that the service remain confidential to counter what she says is a pervasive mental health stigma in the professional medical community.
“Almost every call into the physician support line starts with an apology and that should speak to how it is received that there is an inherent reluctance among physicians to admit they’re struggling and to seek help for that struggle," she said.
Masood also says anonymity helps protect physicians from potential professional repercussions.
“I knew that if anyone was going to be using the Physician’s Support Line ... it had to be made clear that this was not going to be reported to any systemic entity,” she said.
In some cases, doctors and nurses are faced with disclosure requirements about mental health on job and state licensing applications.
While only questions about current impairments are appropriate for licensure under the federal Americans with Disabilities Act, doctors who spoke to ABC News said the nature of some of the questions continues to deter medical staff from seeking help.
According to a 2019 study in the Journal of Psychosocial Nursing and Mental Health Services, more than half of nurse pre-licensing forms complied with ADA rules surrounding mental health questions. However, roughly 40% of nurse licensing questions still probed far beyond the scope of current impairment.
In 2018, only 18 states had physician licensing applications that were ADA compliant, according to the Journal of the American Academy of Psychiatry and the Law.
That same year, the Federation of State Medical Boards released recommendations to reduce the number of stigmatizing questions on licensing applications and promote the mental wellbeing of physicians. Thirty-nine medical boards across the country have updated that language so far.
Dr. Kim Templeton, vice president of the Kansas State Board of Healing Arts, has worked to update the language in her state to meet those standards.
“Physicians can’t help others until they help themselves,” she told ABC News.
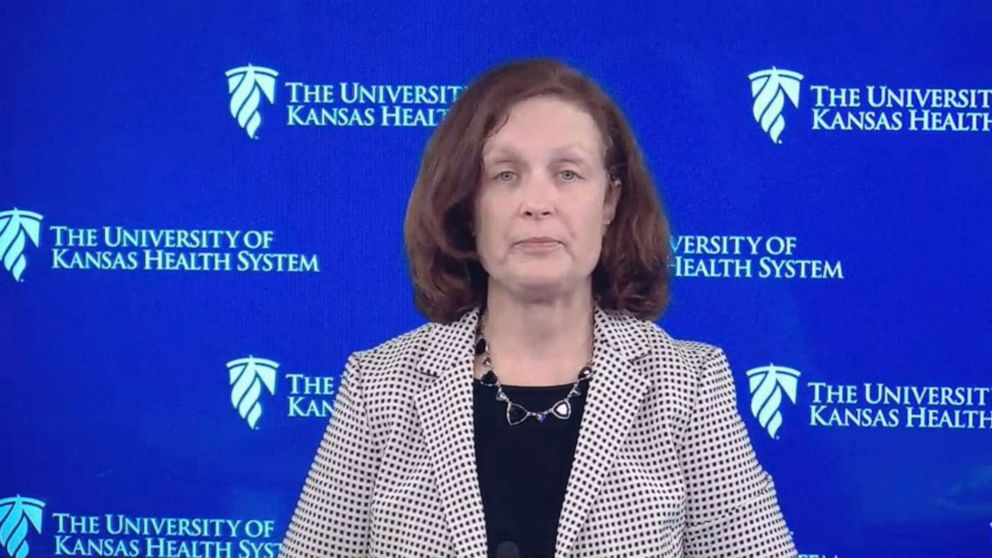
In 2020, Templeton partnered with the American Medical Women's Association to launch the Humans Before Heroes initiative, which aims to help other states update their standards.
“What we’re trying to do is encourage them … and that means removing the hurdles to seek care,” she said.
While New York is one of the few states that doesn’t ask mental health questions on its licensing forms, Breen’s family says the culture within the medical community regarding mental health was crippling.
“She was worried about her license. She was worried about her job. She was worried about the respect of her peers. It was an unsurvivable scenario,” said her sister, Feist.
In a statement, New York-Presbyterian Hospital told ABC News, “[We continue to] mourn the passing of Dr. Lorna Breen. Dr. Breen was a heroic, remarkably skilled, compassionate and dedicated clinical leader who cared deeply for her patients and colleagues. … New York-Presbyterian and Columbia [University] began offering robust mental health services, including an urgent counseling service, to all of our front-line staff in late March 2020. It is essential that our colleagues on the frontlines continue to have access to emotional support and practical strategies to enhance coping.”
Feist and her husband are now working to break stigmas and other barriers to mental health care within the medical profession at the national level. They have co-founded the Dr. Lorna Breen Heroes Foundation and are partnering with organizations and members of Congress to introduce the Dr. Lorna Breen Healthcare Provider Protection Act in an effort to pursue lasting change.
As the one-year anniversary of Breen’s death approaches, Feist said that they've honored her sister and spoken out for others who've been devastated from the pandemic, but that she views these incidents "as an error."
"This was a mistake that could have been avoided," she said, "and I would like to say in my sister’s honor that we are helping other people avoid it.”




