An American tragedy: Inside the towns hardest hit by coronavirus
A South Dakota doctor is moonlighting as a newspaper columnist, urging readers to protect themselves against the virus that killed both his parents.
The sheriff in a Kansas town is fighting for his life in a Denver hospital he was sent to for critical care.
In Georgia, a minister who led up to three COVID-19 funerals a day at the pandemic's height dreads his phone's ringer, announcing more death.
On Thursday, the United States crossed a tragic threshold, marking at least 250,537 American lives lost to COVID-19 since the pandemic's start, according to Johns Hopkins University. After nine months of numbers, it's hard to conceptualize the immense tragedy behind that figure. But we should try.
A quarter million dead.

In different terms, as Dr. Jorge Caballero, a clinical instructor at Stanford Medicine, explained, our current outbreak trajectory is expected to bring the American death toll to 300,000 in less than a month.
"That's as if you took the entire population of St. Louis, Missouri and wiped it off the map," Caballero said.
As the virus has ripped across the country, from densely populated cities on the coasts to the Sun Belt and back up to the heartland, the face of the pandemic has shifted.
Today, rural America is caught squarely in the virus' crosshairs and the impact of the virus is much more widespread than it was in the spring.
As a proportion of the population, rural counties were always experiencing a disproportionately high death toll. A cluster of deaths at a nursing home in a small town has a different effect, statistically and personally, then it does in a large city. But what's changed since the early pandemic is the number of counties that have lost residents to the virus.

To better understand who is dying from COVID-19 in America and where they live, ABC News analyzed U.S. counties with the highest COVID-19 death rates per capita -- a metric used by researchers at Johns Hopkins University of Medicine and the Centers for Disease Control and Prevention (CDC) to measure COVID-19 data. Within four weeks of the first reported death on Feb. 29 in Washington State, 2.3% of the United States's 3,142 counties were averaging at least one COVID-19 death each week. By the week ending Nov. 13, 26.6% of U.S. counties saw at least one weekly death from the virus.
As the pandemic has evolved and spread, those counties are increasingly rural, ABC News found, with the poorest counties that have the fewest health resources bearing the brunt of the burden.
"Rural is older, sicker and poorer," Alan Morgan, CEO of the National Rural Health Association, explained. "There's a higher percentage of people with multiple chronic issues and comorbidities," he said.
"If you throw in that they have the fewest options available for seeking care, it's the worst possible public health setup you could imagine."
The face of COVID-19 death in America is changing
As the first eight months of the U.S. outbreak unfolded, striking disparities emerged.
In addition to having higher rates of infections, counties with majority non-white populations experienced COVID-19 death rates at least three times higher than the death rates in counties in which less than 10% of the population was non-white.
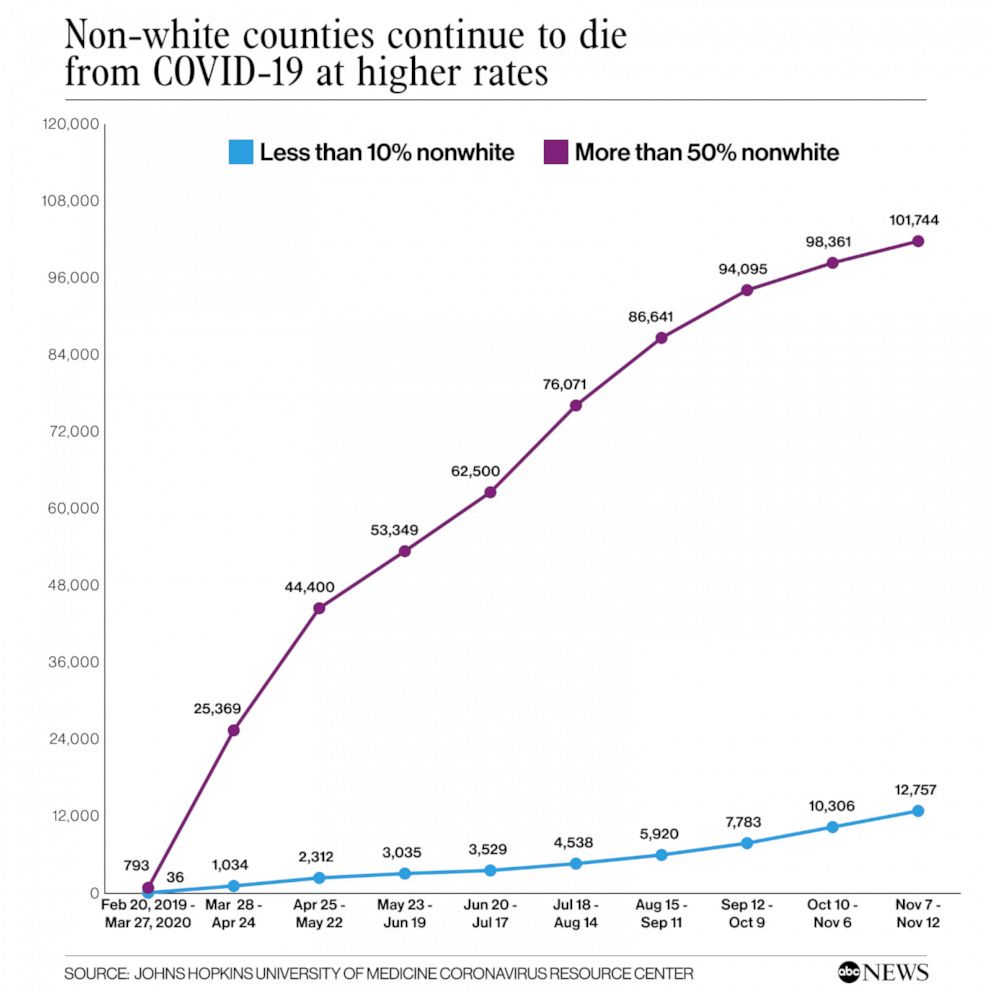
Then in recent months came an explosion of cases in the upper Midwest and Plains states, where most of the population is mostly white, causing deaths to increase at a higher rate in white counties and the disparity between non-white and white death rates to narrow.
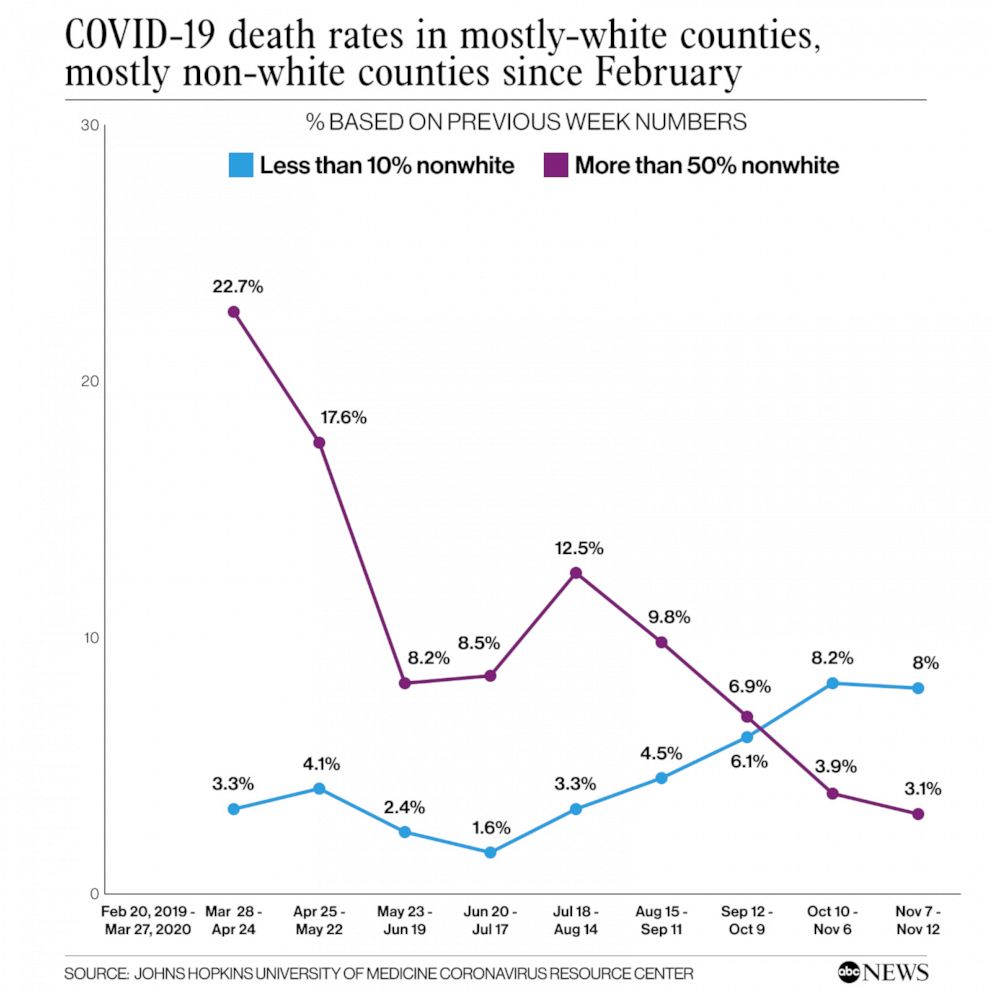
While it's tempting to view the narrowing gap between Black and white deaths as a sign that COVID-19 racial disparities are improving, that's likely a false narrative, according to Theresa Chapple-McGruder, a Washington D.C.-area epidemiologist.
"We’re seeing more of a regional shift than a racial shift," Chapple-McGruder said.
Black and Hispanic people in the U.S. are still disproportionately dying of COVID-19. Black people in the United States were 2.1 times more likely to die from COVID-19 than white people were, according to a CDC report published in August. Hispanic people were 1.1 times more likely to die from the virus.
Where people live in the U.S. is highly segregated by race and deaths are currently spiking in areas with very low rates of Black and Hispanic residents, Chapple-McGruder noted.
The COVID-19 death rate was highest in the Northeast counties over the past nine months, but in mid-summer, the death rate in Southern counties rose by double digits. In the past four weeks, the biggest regional jump in deaths was in Midwestern counties.
"Even in places where we’re not seeing the insane peaks that we’re seeing in the middle of the country, Black and Hispanic people are still overrepresented in the number of cases," Chapple-McGruder said. "Where Black and Hispanic people live, they are going to carry the highest burden."
Terrell County, Georgia, for instance, has four funeral homes, no hospital and one of the worst COVID death rates in the nation. In a place with just 9,000 residents, most of whom are Black and poor, 33 people have died of the coronavirus. Terrell County’s COVID-19 death rate of 383 per 100,000 residents is four times higher than Georgia’s overall rate of 80 per 100,000.
Rev. William Weston Sr. has buried many of them.
If you thumb through obituaries in Dawson, Terrell's biggest town, you'd be hard-pressed to find a funeral that doesn't mention Weston officiating. At the height of the pandemic, he led back-to-back funerals, on several Saturdays two or more. Before a graveside service where he was to eulogize a married couple from his congregation, his phone rang in his pocket.

"For a good couple of months or so, every time I got a call, someone had passed," Weston said. This time the virus struck close to home. The voice on the other end of the line told Weston that his first cousin had died of COVID-19.
When Weston celebrates 17 years as the senior pastor of Sardis Baptist Church next month, it will be the first time his cousin won't be seated in the pew to join in.
"This town was shattered," Weston said of the unrelenting deaths.
Old, sicker, poorer
Early on, as thousands of people in New York City perished from COVID-19, many Americans viewed the virus as a big-city problem.
But as summer transitioned into fall and outbreaks developed in more rural Midwestern states, the narrative shifted. Since mid-July, monthly jumps in death rates in 1,888 rural counties -- those with a majority of population living outside an incorporated city or town -- have outpaced the increases in their urban counterparts, where most of the residents live in an incorporated area.
Geography, it seems, is no match for COVID-19. "Very few places in the country are actual bubbles," said Caballero, who built a national testing directory that the federal government uses as part of its COVID-19 response effort.
Now that the virus has been unleashed in rural America, it's clear just how vulnerable the nation's older, sicker and poorer rural communities are. Problems with the rural health care system have long been documented, as have myriad health issues that Americans in these areas face.

According to an ABC News' analysis, counties in which 10% of residents lacked health insurance reported COVID-19 death rates more than 10 percentage points higher than better-insured areas. "Medically underserved" counties, a designation the Health Resources and Services Administration uses for areas with insufficient primary care providers, high infant mortality, concentrated elderly population, or high poverty, had an overall death rate of 77 per 100,000 residents -- 1.5 times higher than in all other U.S. counties.
Independent of health care, poverty is its own risk factor for a high COVID-19 death rate. In counties where the median household income was below $35,000, the death rate was 1.6 times higher than in counties where household income was higher than $75,000. In the very poorest counties, where a quarter of residents are below the poverty time, the death rate was 2.5 times higher than in richer areas.
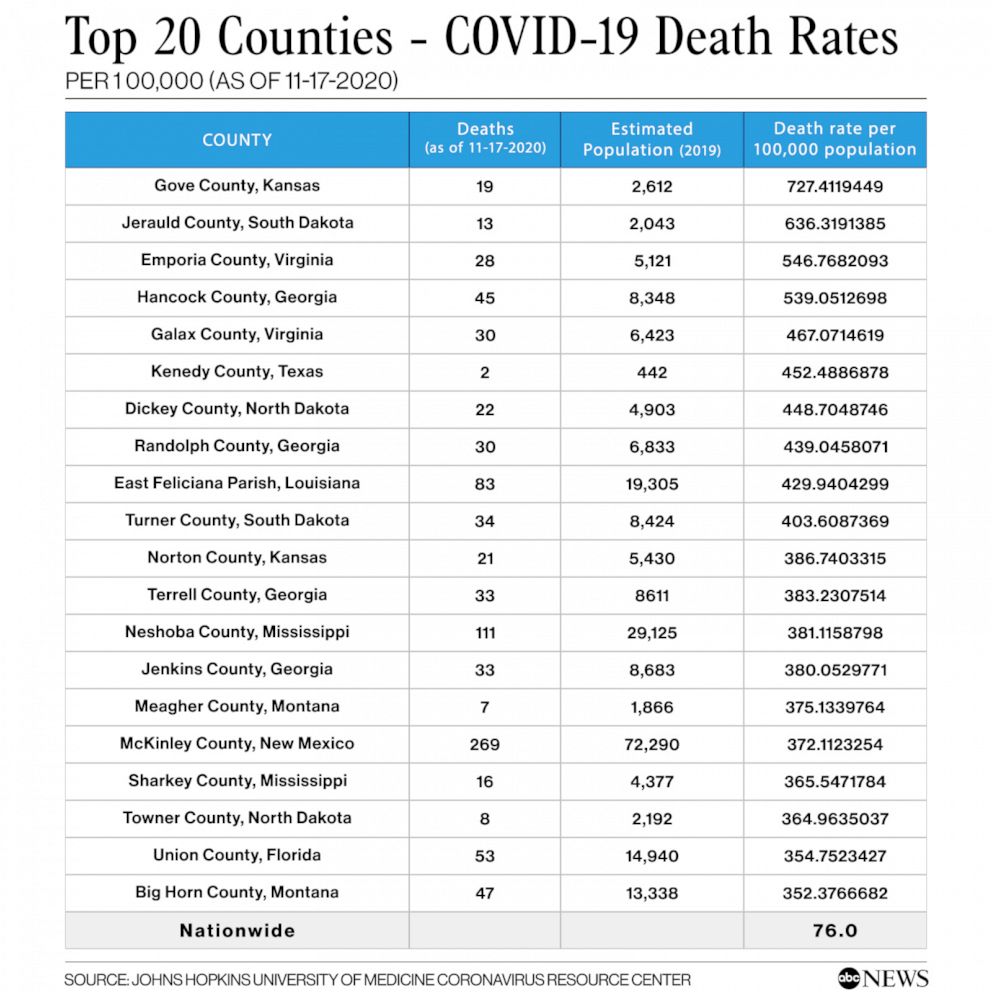
ABC News owned stations reported from hardest-hit counties across the country. Of those counties, Gove, Kansas, stands at the top of the list.
Nineteen people in the 2,600-person county have died of COVID-19 since early October, many of them residents in the local nursing home.
In a small town, even one death has a ripple effect.
"Everybody knows somebody who has died,” said Dr. Doug Gruenbacher, a physician in the county.
The virus has also strained the hospital system, Gruenbacher explained. Rural hospitals rely on transferring out critical patients to better-equipped hospitals and right now, no one has space for his patients, Gruenbacher said. Instead, there’s a waiting list and patients are transferred days later than they otherwise would have been.
"That puts an undue amount of stress on our hospital and our physicians,” he added. "It’s just unnerving to be taking care of a patient and you’re not able to do in the best manner possible for them.”

Among the patients transferred out of state for higher level care was Gove County Sheriff Allan Weber, who struggled with COVID-19 complications for more than a month.
"He’s got tremendous risk factors and it's pretty worrisome,” Gruenbacher said.
For rural doctors, no safety net
It was a "burst of bad events," as Dr. Tom Dean put it.
Dean is one of just three doctors in Jerauld County, South Dakota, where COVID-19 invaded the local nursing home, killing both of Dean's parents.
The county's 13 deaths, largely due to the nursing home outbreak, rocked the 2,000-person community and propelled the death rate to the second-worst in the nation.
"It’s different than anything I’ve encountered over 40 years of practice," Dean said of the virus. "It's invisible, it's silent and sneaks around. It flares up when you don't expect it," he said. "Because of that, people tend to think that it flared up and went away and we’re done with it."
The town is small enough that Dean has also taken on the role of clarifying public health advice for his neighbors in a weekly newspaper column he's been writing for the local newspaper.
"We are in the middle of an outbreak, even when we think we are not," he wrote in The True Dakotan in September.

Accurate public health messaging is just one of several battles rural doctors like Dean are fighting right now.
Hundreds of rural communities that used to have a hospital lost them in recent years. Ninety-five rural hospitals closed between January 2010 and January 2019, according to the Department of Health and Human Services' Federal Office of Rural Health Policy. Of those facilities, 32 were critical access hospitals, meaning they offered 24-hour emergency care services 7 days a week.
The 1,821 rural community hospitals that were still standing this year standing aren't well-equipped to handle critically ill COVID-19 patients and traditionally rely on transferring patients who need ICU care to partner hospitals.
"Rural hospitals are designed for primary care and general surgery," Morgan said. "They were never designed for a global pandemic response." Already the National Rural Health Association's member hospitals are seeing transfer delays in South Dakota and Kansas, he added.
Making matters worse, local health departments were outright gutted over the past decade.
In addition to an 18% drop in spending for local health departments since 2010, at least 38,000 state and local public health jobs have been eliminated since the 2008 recession, leaving behind a skeletal workforce, according to an August investigation by Kaiser Health News and the Associated Press.
The last tool in the toolbox, fundamental public health interventions like masks and social distancing, haven't been embraced in many rural areas.
"What we didn't know back in April was the extent to which these rural communities would not employ public health measures such as mask wearing and social distancing," Morgan said. "Everything that could go wrong is going wrong in these small towns."

Part of that is political. South Dakota is one of the states where the governor declined to issue a statewide mask mandate for residents even as COVID-19 cases, hospitalizations and deaths in the state exploded.
The other piece of the puzzle may be ineffective messaging. Rural counties may not have a designated public health department at all, meaning residents may not have easy access to whatever state or regional resources may be available and often travel long distances for health care and testing.
"They're hearing messages from places they've probably had very little interaction with," Chapple-McGruder said. "When the pandemic was hitting New York and New Jersey really badly, the majority of the country went into a lockdown," she added. "Our national messaging was all the same. That might not have been appropriate for areas with zero cases."
Disillusionment could partially explain why Dean said he has struggled to get his community to take COVID-19 seriously.
"People in more rural areas experienced the pandemic from a policy perspective, but not a health perspective," Chapple-McGruder said. "There was time to build up mistrust in those areas and make it seem as if the pandemic was not real."
Even as loved ones die of coronavirus, that mistrust lives on. Public health messaging just isn't resonating in many rural counties, Morgan said. "It's an incredibly difficult time to be a public health official in rural America."
It's a phenomenon Gruenbacher recognizes. "All of us physicians love our small town. People will bend over backward for you to help you, but those same people are the last ones you can tell to put a mask on,” he added. “They are pretty strong-willed. They don’t want to be told what to do.”
Mistrust and politicization of the pandemic are making life tough for doctors like Dean, who described the political conflict over masks as "terribly unfortunate."
"In too many situations, whether or not you wear a mask has in taken on some kind of political message and that’s totally wrong," he said.
"He’s just beyond frustrated," Morgan said of the doctor and his newspaper column. "He’s a small-town doctor who is trying the best he can to keep this community alive and they are fighting him on it."
ABC News' Jenny Wagnon Courts, Emily Ruchalski and Heather Guzman contributed to this report.
What to know about the coronavirus:
- How it started and how to protect yourself: Coronavirus explained
- What to do if you have symptoms: Coronavirus symptoms
- Tracking the spread in the U.S. and worldwide: Coronavirus map
Tune into ABC at 1 p.m. ET and ABC News Live at 4 p.m. ET every weekday for special coverage of the novel coronavirus with the full ABC News team, including the latest news, context and analysis.




