Research shows promising development in hunt for HIV vaccine
After more than 30 years of attempts, there may be a promising advance in the search for a vaccine for HIV, the virus that causes AIDS if left untreated.
Now, preliminary data from an early stage clinical trial out of the International AIDS Vaccine Initiative and The Scripps Research Institute in La Jolla, California, suggests that a new HIV vaccine may hold promise.
"These are very early studies. But nonetheless, they are provocative," said Dr. William Schaffner, a professor of preventative medicine and infectious diseases at Vanderbilt University in Nashville, who was not involved in the clinical trial.
Although the vaccine candidate will still need to be tested in larger studies, experts are hopeful this vaccine might succeed where others have failed.
"This is a very innovative approach to developing a vaccine that hasn't been done before," Schaffner said, who described the underlying vaccine technology as "kind of a culmination of 21st century science."
When HIV was first discovered as the cause for AIDS in the early 1980s, researchers thought that a vaccine for this virus could be created rapidly, as had been done for diseases like measles, chickenpox and hepatitis B. In fact, the then-U.S. secretary of health and human services, Margaret Heckler, predicted in 1984 that a vaccine would be available in two years. Researchers soon found that there were more hurdles than they had initially thought.
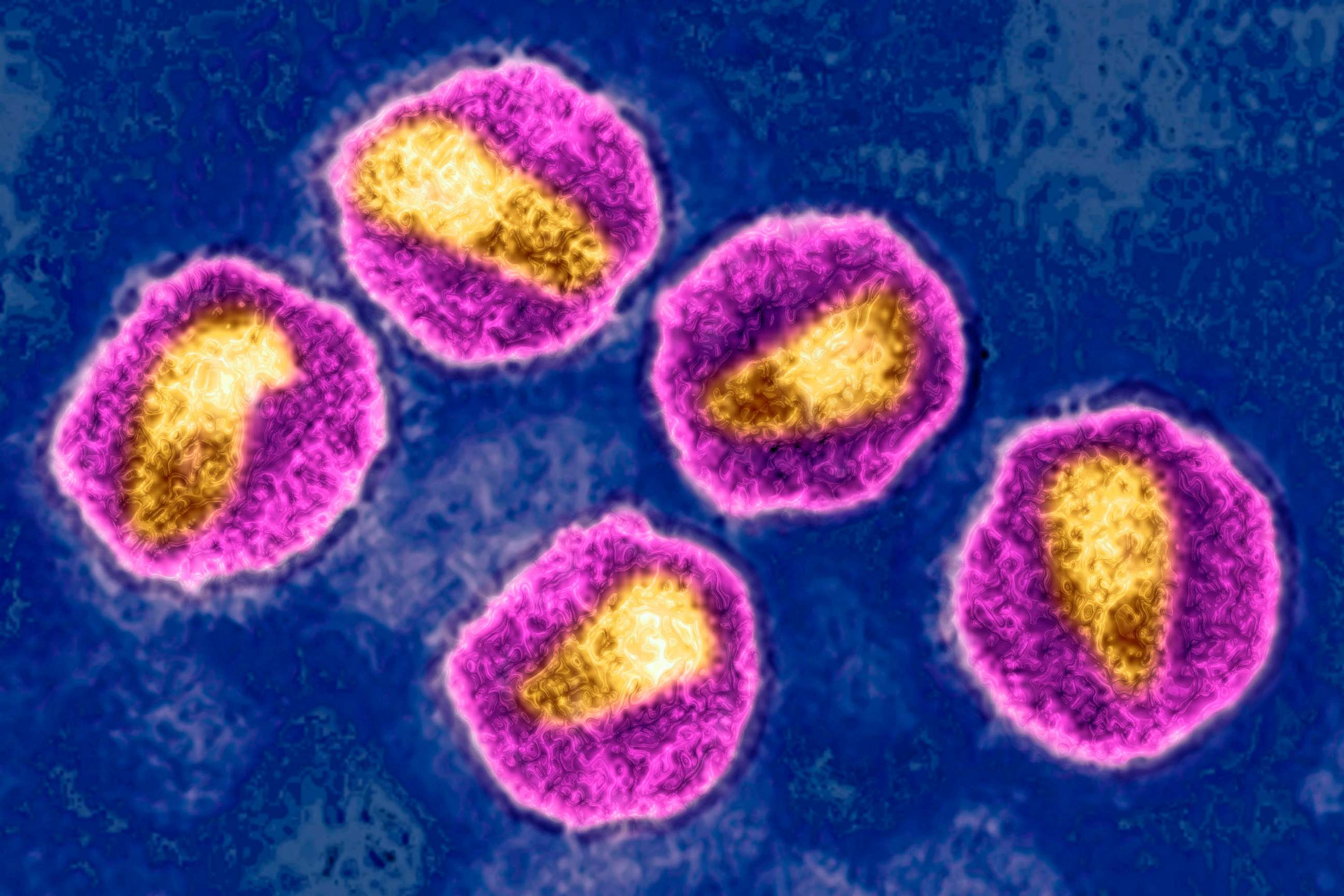
HIV is a virus that mutates rapidly, creating a moving target for vaccines. HIV also has many different subtypes, so a vaccine offering protection against one subtype of HIV may be ineffective against another.
The new research out of IAVI and Scripps aims to address these difficulties by developing a vaccine that helps the body create "broadly neutralizing antibodies." The researchers hope to stimulate a person's immune system against many HIV variants and mutations.
This research is based on "identification of a subset of HIV-infected individuals ... who, in the course of their infection, do make so-called broadly neutralizing antibodies, which basically means these antibodies are able to potently block infection of diverse HIV variants, and that is the key goal," said Dr. Mark Feinberg, Ph.D., the CEO of IAVI.
Their early stage, phase 1 clinical trial, which is still underway, involved 48 healthy adults who received a total of two doses of either the vaccine or placebo, two months apart. Preliminary data showed 97% of those who received the vaccine had early evidence that their immune system may be able to make these broad antibodies.

"The broadly neutralizing antibody is important, because the virus can mutate so rapidly that they need something that's a shotgun, not a rifle ... to prevent a whole variety of different kinds of HIV configurations," said Schaffner.
The decadeslong search for an HIV vaccine lies in stark contrast to the development of vaccines for COVID-19, "where the science was ready, and we were able to develop vaccines, plural, very, very quickly," Schaffner added.
The researchers at IAVI and Scripps are collaborating with companies, like Moderna, to harness the mRNA technology used in the development of vaccines against COVID-19. While the candidate HIV vaccine being studied in this trial is not mRNA based, the researchers are looking at how mRNA technology may be used in the future to further development of an HIV vaccine.
Sara Yumeen, M.D., is a preliminary-year internal medicine resident at Hartford Healthcare St. Vincent's Medical Center in Connecticut and is a contributor to the ABC News Medical Unit.




