India has few coronavirus cases, but the country is unprepared for a spike, experts warn
LONDON and DELHI -- Earlier this week, the prime minister of India, Narendra Modi, announced that the lockdown currently in place to protect 1.3 billion people would remain in force until at least May 3.
While the lockdown has been partially lifted in rural areas for economic reasons, the scale of the fundamental changes to life in the world’s largest democracy, with Indians told to stay inside no matter what the circumstances in order to maintain their social distance, is almost beyond comprehension.
As of April 16, only 10,541 confirmed coronavirus cases and 423 deaths have been recorded -- a relatively small figure in comparison to the total population -- and to the outside world it may seem that India is coping.
Yet the size of the lockdown is only matched by the potential for COVID-19 to wreak havoc on India’s healthcare system. With poverty, overcrowding and hospitals working at full capacity during the best of times, experts and doctors are warning that the coronavirus pandemic could easily overwhelm the healthcare system, should there be a spike in cases, like the ones that have stretched those in Europe and U.S to their very limits.
‘A possible recipe for disaster’
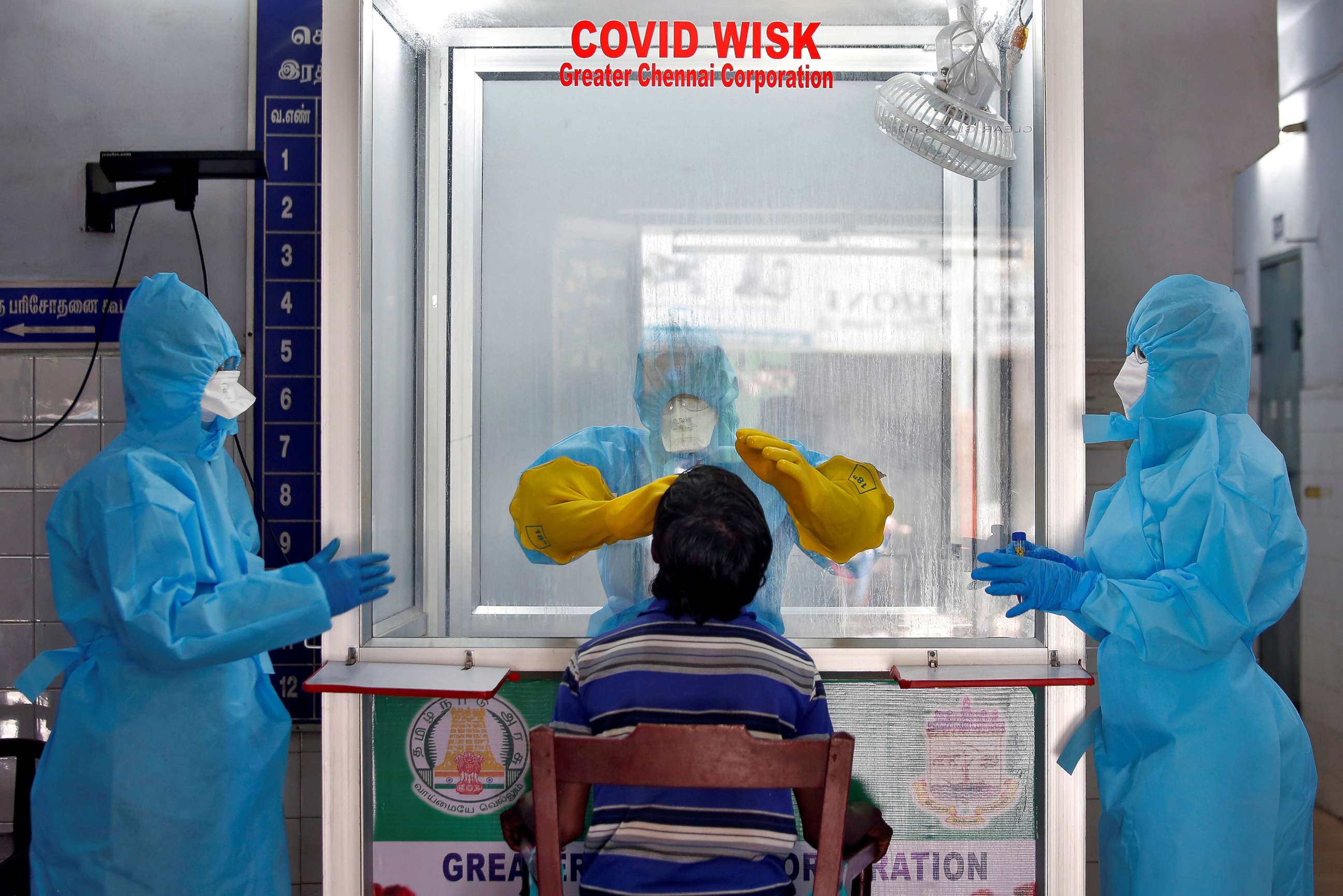
Last month Dr. Srinavas Rajkumar, the general secretary of the Resident Doctors’ Association at the All India Institute of Medical Sciences (AIIMS), one of India’s top public hospitals based in New Delhi, directly appealed to Modi for better equipment for frontline doctors. In the video, he described harrowing conditions for the medical workers dealing with India’s nascent coronavirus epidemic.
“I, along with many other doctors here, and all over the country, are deployed in COVID duty with either insufficient or inadequate Personal Protective Equipment,” he said. The equipment provided failed to meet worldwide safety standards he said, although doctors were continuing their duties “in spite of the imminent threat to themselves.”
Rajkumar is painfully aware of the task Indian doctors are facing with the pandemic, even as more healthcare systems in more developed parts of the world struggle. Some of the PPE doctors were provided simply look like "raincoats," he said.
"Indian healthcare always works at more than the capacity,” Rajkumar told ABC News. “Every major government hospital handles more patients than they are meant to handle, even on a regular day."
Though he received no official response to the appeal, the quality and availability of PPE have since improved, he said.
But India’s healthcare system appears to be especially vulnerable to a virus that seems to spread quickly through populations, particularly in crowded urban areas and an unregulated countryside.
A “best-case scenario,” the director of the Center for Disease Dynamics, a public health research organization with offices in Washington and Delhi, said, would be 200 million infections.
For a country of its size, India has an alarmingly low rate of doctors, by any reasonable metric. According to the latest statistics from the World Health Organization, the country has less than 0.8 doctors per 1,000 of the population. The United States has triple that amount.
According to an analysis from the Brookings Institute, a think tank, of publicly available data, there are 0.55 beds per 1,000 of the population in India nationwide – a number they described as “abysmally low.” China, the only country comparable country to India in terms of size, has around 4.2 beds per 1,000 people, according to World Bank data.
While there is no publicly available data on the number of ventilators in India, Brookings estimates that there are between 17,800 and 25,600 ventilators in ICU wards there. Meanwhile, there are roughly between 150,000 – 200,000 ventilators in the United States, and even that number is believed to be well short of what is required to deal with the pandemic.

India has plenty of history when it comes to pandemics. Periodic outbreaks of dengue fever have overwhelmed local health authorities in recent years, according to Rajkumar. And the country was particularly hit by the last global pandemic comparable to coronavirus, Dr. Elizabeth Chatterjee, a lecturer in regional and comparative politics at Queen Mary University in London, told ABC News.
“Much of this fear is based on the memory of the so-called "Spanish flu" of 1918–19, when perhaps 18 million Indians died (6% of the population at the time), the largest death toll in the world,” she said. “Indians today are much healthier and better governed than in the colonial era. But still the country's sheer density makes mass transmission dangerously likely, especially because 160 million Indians still lack access to clean water to wash their hands.”
“Add to this India's high levels of air pollution and underlying health conditions like diabetes, and it is a possible recipe for disaster,” she said.
According to IQAir's latest World Air Quality report, India is the world's fifth most polluted country, and is home to 21 of the world's 30 most polluted cities.
There are, however, some factors which mean India may be less vulnerable to the virus, as the "younger age of the population is a protective factor," compared to other hard-hit countries, according to Dr. Srinath Reddy, the President of the Public Health Foundation of India.
What to know about Coronavirus:
- How it started and how to protect yourself: Coronavirus explained
- What to do if you have symptoms: Coronavirus symptoms
- Tracking the spread in the U.S. and worldwide: Coronavirus map
'You can only imagine'
The Indian government has boasted that the country "has managed to significantly contain COVID-19 as compared to other severely hit countries."
But testing so far has been "grossly inadequate," according to Rajkumar.
"The percentage is very, very minuscule," he said. "It is very important to note that without adequate testing, the likelihood of getting real figures is very low."
India has among the lowest testing rates in the world, according to Chatterjee. That means that an accurate understanding of how far the coronavirus has already spread is difficult to come by.
“The Hindu nationalist government has prioritized testing cases around the Tablighi Jamaat, an Islamic group that held a large event with many foreign visitors in Delhi last month,” Chatterjee said. “In this way, the statistics fan the idea that COVID-19 is transmitted by foreigners and Muslims, though it is clear that there has been community spread for weeks.”
For the time being, however, hospitals across the country have not yet seen an overwhelming spike in admissions associated with COVID-19, according to Dr. Srinath Reddy, the President of the Public Health Foundation of India.
“It is true that it [up to] 270 odd districts have reported cases,” he told ABC News. “But hospitals are not bearing a severe load like in Europe or America and elsewhere, so that suggests that the viral spread is not that rapid.”
However, the key test will be the impact that the lockdown of the whole country -- now in place until early May -- has on the transmission of cases.
“We still have to wait one or two weeks to find out whether there is going to be a rise in cases,” he said.
Even at this early stage, however, there are signs that the health infrastructure is creaking under the pressure. The Delhi State Cancer Institute temporarily shut, and has since reopened, after a number of doctors tested positive for the virus earlier this month, according to local media reports. The same temporary closures after COVID-19 diagnoses have happened in other hospitals in Mumbai and Delhi.
The re-allocation of already “scant” resources to deal with the pandemic, in a country where waiting lists for crucial treatments for diseases like cancer stretched for months even before the pandemic, will likely have a deadly cost, according to Rajkumar.

"Regular doctors are shunted to COVID care," he said. "If that's the case on a normal day, then imagine now."
The problem of lack of resources is especially acute in rural areas. Around two-thirds of the Indian population live in the countryside, and it is not uncommon for people to travel hundreds of miles for critical medical care in the better equipped urban hubs of Delhi and Mumbai. People in the further-flung regions of India dying without seeing a doctor is a fact of life for many, and could be obscuring the true scale of the coronavirus in India thus far.
"There are places in rural India completely inaccessible to healthcare and testing facilities, even without the pandemic in India there are people dying without access to healthcare facilities,” Rajkumar said. “There are people traveling aboard trains overnight to reach Delhi to get treatment. Due to lockdown, there are already reports that [people] are dying of causes other than coronavirus… you can only imagine what would be the state in rural India."
The need for change
A key pledge of Modi’s ruling government was to implement ‘Modicare,’ which would provide health insurance for up to half a billion of the poorest Indians. However, the reforms are yet to fully take hold across the country, with only 20% of those eligible covered by the program as of December 2019, according to Reuters.
“We have shortages everywhere,” Dr. Reddy said. “That’s really where we need to invest much more in expanding and skilling – both scale up and skill up of our workforce.”
Yet the lack of a centralized system – with health policy determined on a state-by-state basis, means some states, particularly in the south of the country, are in a better position to deal with the pandemic.
“Public healthcare in India rarely functions as a ‘system,’” Dr. Anna Ruddock, a medical anthropologist specializing in India, who is authoring a book on the link between medical education and health inequalities in the country. “As important as overall scarcity is uneven distribution. Public healthcare is inadequate everywhere, but the services that do exist are heavily skewed to cities.”
“While the pandemic response is being centrally directed, health in India is the responsibility of individual states - we see disparities in terms of preparedness and responsiveness playing out very clearly, with direct consequences for the lives of citizens,” she said.
In terms of distribution, the “northern states will suffer most,” according to Rajkumar. The authorities in southern states, some of which have "very good public healthcare," are for the most part better prepared for the pandemic, where the number of medical colleges and hospitals is comparatively high, he said. In Kerala, the authorities even claim to have flattened the curve.
Nationwide, public health, unlike in the U.S. and U.K., has “never been a political priority in India,” Ruddock said. But there is a chance that the pandemic may lead to sweeping changes for the better.
“India’s health system certainly requires a major revamp in terms of the total amount of public financing, expansion of its health workforce, strengthening of its primary healthcare district hospitals and reducing the inequalities that lay in health system preparedness and deficiency between the various states,” according to Reddy. “And we are hoping that the lessons learned from this won’t be forgotten when COVID-19 is quelled.”




