Immunity to COVID-19: Front line health workers consider deliberate infection
As COVID-19 numbers climb precipitously, health care workers, first responders and the countless individuals working in "essential services" make a heroic decision: Do I come to work and put myself and my family at greater risk, or do I #StayAtHome? This decision is made harder by ongoing shortages of necessary personal protective equipment.
As cases grow, the likelihood of each one of us contracting COVID-19 grows with it. Some front line workers have started to question if getting COVID-19 now would help them become immune, so that they can better cope with PPE shortages and higher threats of exposure.
Those with suspected exposure to COVID-19 only have interim guidance for what to do. The CDC recommends that those who can get tested should only return to work if they have no fever without the help of any medication, have improvement in their breathing or other respiratory issues, and have two negative swab tests at least 24 hours apart. Those who cannot get tested have to wait at least 72 hours after their last fever without medication and have at least seven days of improved symptoms. And when they do return, they should consider wearing a face mask.
Clearly, it would be ideal if healthcare workers could find some way to become immune to this virus. Since a vaccine is more than one year away, some are considering exposing themselves early on, gambling they will be a member of the lucky majority with mild symptoms. Maybe they’re on to something?
Unfortunately, it’s much more complicated than that.
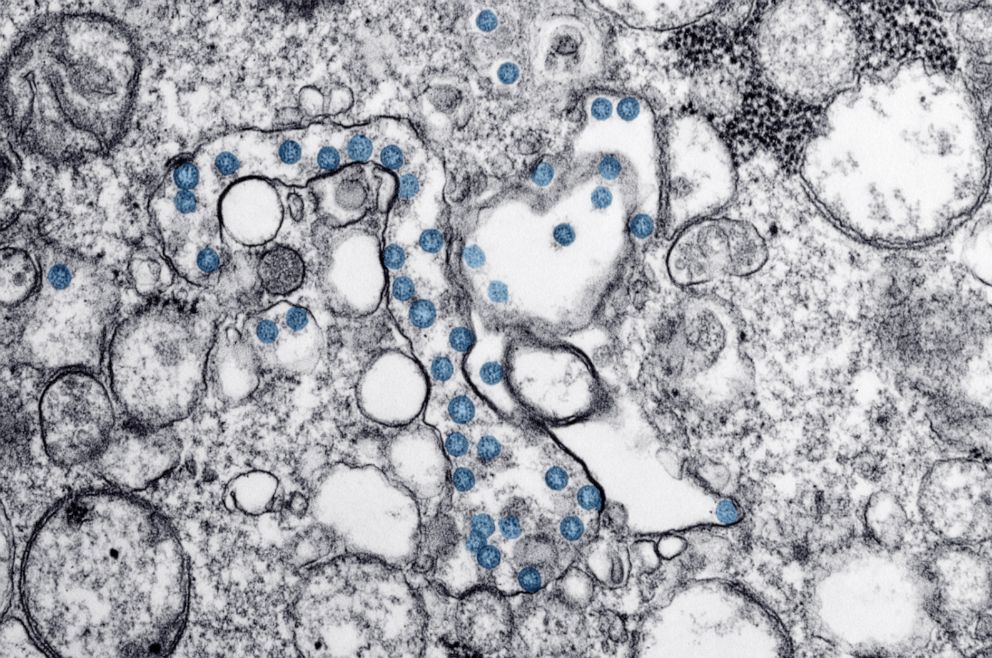
Immunity is an intricate and convoluted experience for your body, and we are only in the infancy stages of understanding the immune response to COVID-19. How your immune system gets activated, the length of activation, the magnitude, how it spreads, and whether it stays present in different parts of your body can all differ based on the virus. This may mean that immunity may be temporary, if it exists at all.
That being said, speculation that the body will build immunity to COVID-19 exposure is reasonable. In fact, a mild exposure to a germ or virus prompts your body to launch germ-fighting tools (macrophages, B-lymphocytes, T-lymphocytes, etc.). After the infection, the immune system remembers what it learned and is able to defend against another attack.
In essence, that is how vaccines work. So, whether through exposure or vaccine, if our bodies build immunity, we may be able to protect our front line now, and eventually protect everybody -- a concept referred to as herd, or community, immunity.
What to know about Coronavirus:
- How it started and how to protect yourself: Coronavirus explained
- What to do if you have symptoms: Coronavirus symptoms
- Tracking the spread in the US and Worldwide: Coronavirus map
Until we know more about COVID-19, scientists have been comparing this virus to others that we know better, such as SARS and MERS. A similar virus, MERS, does appear to give patients immune protection after they recover, but according to the CDC, “It is not yet known whether similar immune protection will be observed for patients with COVID-19.”
Herd immunity
Dr. Todd Ellerin, the chief of infectious disease at South Shore Health, in Massachusetts, advocates for herd immunity. “What stops a virus, what breaks the chain, is if enough people get infected and those people develop immunity. In fact, if enough people get infected, the virus can’t replicate in that host. … If you have immunity, you can’t get infected because the antibodies swarm like an army.”
Herd immunity would mean that enough people have an exposure that then protects people who either would be at high risk or can’t get vaccinated once one is approved.
If immunity is probable, some have proposed that we all become infected now so that we'll be immune later. But we still don't know enough about the way the virus works to know if this is a good idea. Although we still don't know exactly what percentage of people who get infected die of COVID-19, we do know that if everyone stopped trying to protect themselves from infection, it's likely that tens of thousands of Americans would die.
Dr. Simone Wildes, an infectious disease specialist also from South Shore Health, cautions, “It’s just too early for us to say. We think about when we get a cold, and then get another cold, it’s no big deal, but we don’t know with COVID-19.”
Additionally, while you may develop immunity to one strain, you may not have protection against the other. “Just like with influenza A and B, you can get both, getting one doesn’t protect you against the other, so you still need to take necessary precautions, you need to protect yourself and others," she adds.
For now, it seems, risking intentional exposure, or assuming full immunity from a previous exposure, is premature. This leaves the front line back at the drawing board. Do they continue to don hard to find PPE that may be reused or inadequate?
So why the premature push toward herd immunity? Even if mass exposure has the potential of herd immunity, we are completely ill prepared as a nation. It's much better to develop herd immunity using a safe and effective vaccine than by exposing yourself to a virus. That's what we do every year for viruses such as influenza.
When the majority are immunized, those who cannot be -- infants, people who are immunosuppressed, etc. -- are protected. But unlike influenza, we are not equipped with a vaccine for COVID-19. There is no known or approved medication to treat the symptoms in people who are already sick. We are already overwhelming hospital systems in regions with high cases of COVID-19, and we are threatened by the lack of sufficient PPE. Launching an effort to expose the masses intentionally could be catastrophic. It would be a better consideration when we have those measures in place, so we can safety handle the influx of new cases.
Potential government shift in strategy
These warnings may not deter a shift in strategy by the government. Late on March 22, President Donald Trump tweeted, “WE CANNOT LET THE CURE BE WORSE THAN THE PROBLEM ITSELF. AT THE END OF THE 15 DAY PERIOD, WE WILL MAKE A DECISION AS TO WHICH WAY WE WANT TO GO!” leading to speculation that the economic impact would be prioritized over the pleas of scientists and clinicians worldwide.
During the daily briefing on the coronavirus at the White House on Monday, Trump said our country was not built to be “shut down,” and that “this was a medical problem, we’re not going to let it turn into a long-term financial problem.”
Resolution of this pandemic cannot ride on hopes of herd immunity that have not been substantiated by science. The nation is not prepared for the consequences.
Delaram J. Taghipour, M.D., M.P.H., M.B.A., is a preventive medicine resident at Johns Hopkins Bloomberg School of Public Health, and is a contributor to the ABC News Medical Unit.