COVID burden shifts to younger Americans with older generations vaccinated
With vaccination totals increasing and coronavirus cases declining across the country, many Americans are feeling a newfound sense of hope, that perhaps, there is finally a light at the end of the tunnel.
However, health and government officials across the country are continuing to warn that the virus is still spreading among unvaccinated populations, with a larger share of younger Americans becoming infected, and in some cases, hospitalized with severe cases of the virus.
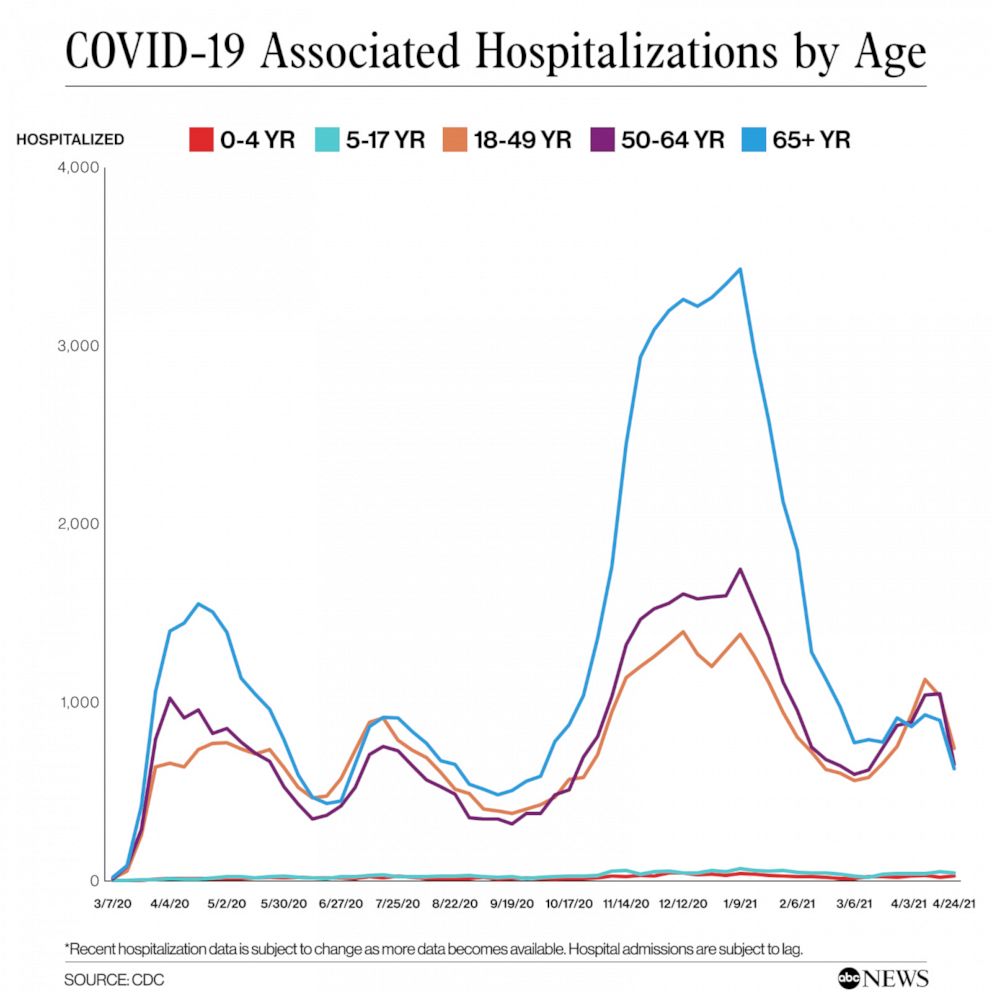
For the first time, patients between the ages of 18 and 64 now account for the largest cohort of the 37,000 total patients currently hospitalized with the virus. With more older Americans vaccinated, this marks the third week that the number of hospitalized individuals in the 65 and older age group has been smaller than both the 18-49, and the 50-64 age groups.
“Hospitals are seeing more and more younger adults, those in their 30s and 40s, admitted with severe disease," Centers for Disease Control and Prevention (CDC) Director Dr. Rochelle Walensky reported during a press briefing earlier this month.
Experts say the exact reason behind this trend is unclear, but could include the rise of variants, relaxed attitudes towards distancing and other mitigation measures, a younger population that is not yet fully vaccinated and vaccine hesitancy. It could also be merely more younger people getting the disease.
Even though not all hospitalizations are the result of severe illness, state officials say the trend is worrying.
“There is a very sharp increase, it appears, in younger adults… these are largely people who think that their age is protecting them from getting very sick from COVID-19, that is not happening,” Cassie Sauer, CEO and president of the Washington State Hospital Association, said during a press conference on Monday.
'Mind-boggling'
Dr. Chris Baliga, an infectious disease physician from the Virginia Mason Franciscan Health in Washington state, reported earlier this week that he has seen more patients under the age of 40 than at any other time in the pandemic, while noting that these younger patients appear to be coming in sicker than before.
“40% of our cases were under the age of 40, which is mind-boggling to me. We never saw that earlier in the pandemic,” Baliga said during a briefing on Monday.
This trend, according to experts, may be the result of a number of factors.
Dr. Katie Sharff, an infectious disease expert at Kaiser Permanente, told ABC News that one of the driving factors may be simply more young people are becoming infected, and with that, inevitably, there will be more severe cases.
While earlier in the pandemic, the disease was affecting predominantly older adults, currently, coronavirus infections among Americans 18-54 account for the highest proportion of new cases per 100,000 residents.

Sharff, too, said she has seen more patients in her Oregon hospital between the ages of 40 and 50 requiring hospitalization, with some patients as young as 30 ending up in the ICU, and a lower percentage have had to be placed on mechanical ventilation.
In Oregon, daily COVID-19 cases have doubled, and the number of patients hospitalized with the virus has surged by 106%.
“If you have that many more young people getting infected there will at least be a subset who develop severe disease,” Sharff explained. Although some patients have pre-existing medical conditions, like obesity, what has been “really striking with this surge” is that not all younger patients needing care have concerning medical conditions that put them at high risk.
Part of the problem, Sharff said, is that younger people, when infected, tend to stay home a bit longer to manage their symptoms, as opposed to older Americans, who generally have been hospitalized earlier in their illnesses.
Because the U.S.’ vaccination strategy targeted high-risk individuals by age, almost all of these younger hospitalized patients have yet to be vaccinated, Samuel Scarpino, epidemiologist and assistant professor at Northeastern University, told ABC News.
“In previous surges, the majority of our patients were elderly and had chronic medical conditions. We're seeing less of that very elderly population and I think that really speaks to the efficacy of the vaccines,” Sharff noted.
Earlier this month, all 50 states opened vaccinations to residents 16 years and older, but it will take some time for those younger populations to be fully protected, Scarpino explained.
“With the 4 to 6-week delay between first dose and the full level of immunity, it will be a few more weeks before those age groups have the same level of protection as older individuals who were vaccinated in months prior,” Scarpino said.
Vaccine hesitancy, pandemic fatigue and variants
But there are other younger people who have chosen not to get vaccinated, Sharff said. “I think that vaccine hesitancy is pretty real,” Sharff noted.
Vaccine demand has been steadily decreasing in recent weeks, as those who were eager to be inoculated get their shots and officials work to convince those wearier to be vaccinated.
Just in the last seven days, the average number of vaccines administered has dropped by nearly 12%, down from the average of 3.3 million doses administered a day, earlier this month, to 2.6 million on Thursday.
According to a recent ABC News/Washington Post poll, nearly 1 in 4 Americans, 24%, are disinclined to receive any of the coronavirus vaccines, down from 32% three months ago. 16% of those polled ruled out vaccination entirely.
Additionally, more transmissible and potentially deadlier variants now account for the majority of new cases across the U.S. The national prevalence of B.1.1.7, first identified in Britain and now, is now estimated to account for nearly 60% of new cases, according to the CDC.
Baliga said he believes the rise of coronavirus variants, and in particular, the B.1.1.7 variant, first identified in the United Kingdom, is behind the rise in cases and hospitalizations among younger people.
“I think that’s what’s driving a lot of what we’re seeing in the younger population,” Baliga said, saying he viewed it as the “single most important” factor driving up numbers.
With more people are succumbing to “pandemic fatigue," and thus letting down their guard, with lax social distancing and COVID-19 protocols, experts say, with many also blaming their infection on increased social gatherings and travel.
Moreover, the combination of more infectious strains of the virus with lower vaccination rates have made young people more vulnerable to the virus.
In Massachusetts, coronavirus variants appear to be hitting younger people more seriously than earlier strains of the disease last year, with an increasing number of residents in their 20s-50s hospitalized, Gov. Charlie Baker said during a press conference on Monday.
While the risk of COVID-19 related death among young populations remains lower than among older age groups, Baliga reported that there are still some young patients who are succumbing to the virus, which he calls a “preventable disease” with vaccines, he said.
To date, over 86,000 Americans between the ages of 18 and 64 have died due to COVID-19, accounting for approximately 19.4% of the U.S. virus-related death toll.
Younger people, in particular, can harbor the feeling that they are less vulnerable to the disease than the more at-risk older adults, Sauer said, but they shouldn't assume that they are “safe from this disease.”
“Our best way out of this pandemic is to get vaccinated," Sharff said. "We are all so exhausted, myself included, but like when you see young people in the hospital dying, you just have to kind of face it head-on and say this is real. We have got to get vaccinated."
ABC News' Brian Hartman contributed to this report.




