

When David Bookstaver tested positive for COVID-19 he happened to have a telehealth consult with his doctor already scheduled that day, to talk about going on medication to moderate his high blood pressure.
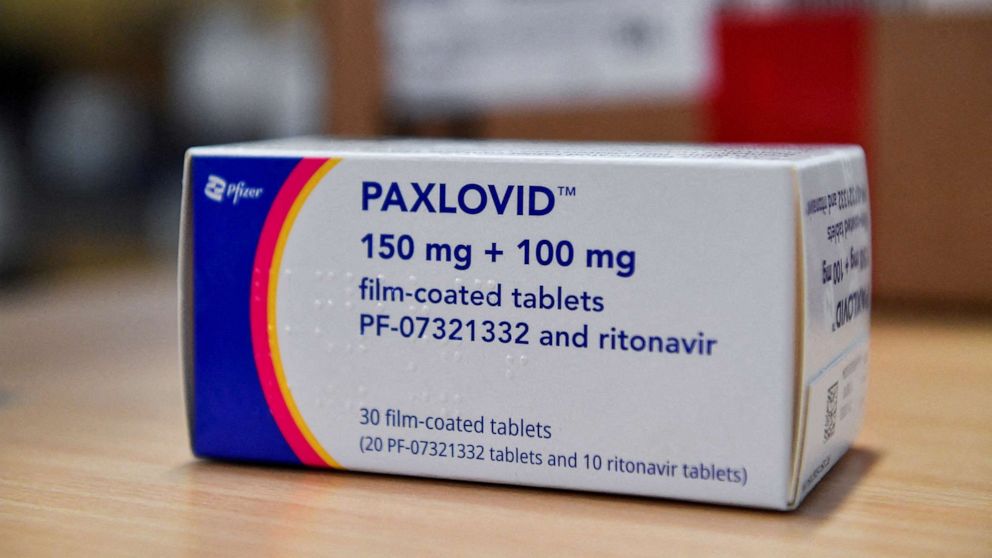
On that call Bookstaver, 63, says his doctor mentioned his age and hypertension made him eligible for Paxlovid, Pfizer's antiviral pill treatment, which has proven highly effective at keeping higher-risk patients out of the hospital, and preventing them from getting even sicker.
Bookstaver is fully vaccinated and boosted and didn't feel too ill at the time – but warding off a turn for the worse seemed prudent. The doctor sent a prescription for the new medication to the pharmacy and his wife was kind enough to pick up his medicine and bring it home.
MORE: Looming COVID drug cuts prompt plans to reclaim, redistribute unused supplyBut when he read over the drug information, Bookstaver's eyes caught on some of the fine print: the cholesterol medication he was already on – and the blood pressure medication he had also just been prescribed – were both listed as having potentially harmful interactions with the Paxlovid he had just been given.
"If I was really sick I probably would have gobbled the first dose up and not looked," Bookstaver said. "I think most people don't do due diligence. They trust their doctor implicitly. But if people aren't checking the contraindications labels I think they kind of need to be told."
Though highly effective, Paxlovid, like some other medications, does carry the risk of certain dangerous interactions with many other commonly prescribed drugs – including those which manage heart conditions and cholesterol. It is also not recommended for patients with severe kidney or liver problems.
"If we're seeing increased concentrations of a statin, this could lead to muscle aches that then lead to impaired kidney function." Dr. Jay Bhatt, an internal medicine physician and instructor at the University of Illinois School of Public Health and an ABC News contributor said. Complications like these, he said, often require hospitalizations for close monitoring.
Without knowing exact medication dosages it's difficult to say just how dangerous potential side effects could have been, but Bhatt, who was not involved in Bookstaver's treatment, said it's a good thing it was caught by the patient beforehand.
As for the blood pressure medications, "we would be concerned about people's blood pressure going so low that we're not getting enough blood flow to the parts of the body that need it. People can pass out and fall. For old patients with comorbidities, that could have serious complications," Bhatt said.
"Some drugs come with more considerations than others -- the prescribing of this particular drug is complex, and it requires a lot of care," Dr. Inga Lennes, senior vice president of ambulatory care at Massachusetts General Hospital, told ABC News. "There has to be a nuanced discussion between a doctor and a patient to make that determination about what is best and safest for your health: talking about not just about their true medication history, what they're on -- but also why they're on it -- is so important."
The drug's tangle of contraindications poses a treatment protocol catch-22: a patient's qualifying risk factors that qualify them for Paxlovid may mean they're already taking other medications for those risk factors which disqualify them for Paxlovid, experts said.
Pfizer told ABC News in a statement it is working to educate healthcare providers on how to manage "potential drug to drug interactions."
"We are also working with some of the largest telemedicine companies to ensure their HCPs are knowledgeable about PAXLOVID and ready to treat appropriate patients, and we are reaching out to pharmacy customers directly to help address questions," the company said.
Bookstaver said he chose not to use his prescription.
This shifting terrain of COVID treatments makes it all the more crucial for doctors to be aware of their patients' full medical profile before signing off on a new prescription, experts said, since there may be potential harms in shifting around their usual drug regimen. And because a prescribing physician or pharmacy staff member dispensing the pills may not be familiar with the full gamut of drug interactions, they said it also underscores the importance of people advocating for their own health and being watchful of how their medicines interact.
"This is not a quick conversation like -- oh, you're COVID positive? You're a certain age? Here, here's your prescription," Lennes said. "We've employed a real massive education effort to make sure that our people who are prescribing these really understand -- there are some drugs that are very specific, they can only be given in certain situations for certain things and under certain circumstances, and it would be dangerous or unwise or unhelpful to prescribe them in any situation.
"All of those micro decisions add up to complexities both for providers and for patients that are hard to navigate and make it harder to automate," Lennes said.
MORE: 4th COVID shot authorized by FDA for everyone over 50Paxlovid's unique effect comes from the synergy of its two antiviral components. One part blocks the enzyme that breaks down the antivirals, leading to high levels of both medications in the body. A long list of other common medications use this enzyme, too – like the statins Bookstaver had already been taking.
The blood pressure medication he was set to start that same day, Amlodipine, is another one that uses these liver enzymes. These typically benign medications effectively become overdosed when taken with Paxlovid.
"Usually the adverse effects are an extension of what the drug is used for. For medications used for your blood pressure, you can have an interaction when your blood pressure gets way too low, dangerously low", Dr. Stephanie Widmer, an emergency medicine physician and medical toxicologist, told ABC News. As for statins, "there is the risk of liver injury, and there's the risk of severe muscle injury and breakdown, which could then lead to kidney injury."
The Food and Drug Administration's fact sheet on Paxlovid notes an extensive list of drug-drug interactions for health care providers, noting "caution is warranted" with Amlodipine, that "clinical monitoring of patients is recommended" and a dose decrease of the blood pressure drug may be needed if co-administered with Pfizer's COVID pill.
Some of these interactions are absolute contraindications and must be stopped, while others are minimal and considered relative interactions, experts told ABC News.
In some cases a patient can pause their other treatments while they're taking the COVID antiviral – three Paxlovid pills twice a day for five days. But for some patients, forgoing the other lifesaving medicines they're already dependent on for a full business week may asking the impossible.
"No matter what medications you're on, because the list is so long, you have to have the conversation with your doctor on if this is the right medication for me and what interactions am I at risk for," Widmer said.
If dangerous drug interactions are unavoidable, doctors may recommend the antiviral pill from Merck instead, called molnupiravir, which has shown to be somewhat less effective than Pfizer's but does not have any known medication interactions. However it is not authorized for people under 18, out of concerns it may impact bone and cartilage growth, and it is not recommended during pregnancy.
"I don't think most people spend the time reading the fine print," Bookstaver said – adding, he's glad he did. "And especially if a person feels bad, they just want to feel better."
ABC News' Eric M. Strauss and Sony Salzman contributed to this report.
Y. Jay Lin, M.D., is an emergency medicine resident at NYU & Bellevue Hospital in New York and a contributor to the ABC News Medical Unit.